Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Congestive Heart Failure (CHF)
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Colin Tidy. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Heart failure does not mean that your heart is going to stop at any minute. It means that your heart is not functioning as well as it should. Heart failure can be caused by many different conditions. Symptoms include fluid retention, breathlessness and tiredness. Medication can usually ease symptoms and can often improve the outlook.
How does the heart work?
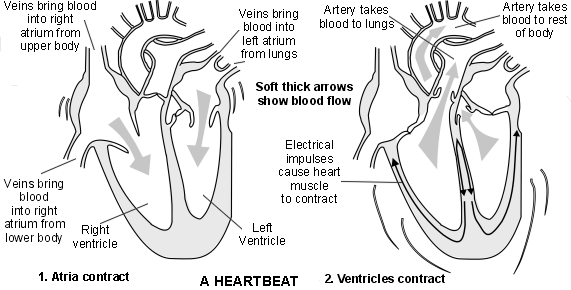
The heart has four chambers - two atria and two ventricles. The walls of the heart chambers are made mainly of special heart muscle. Each heartbeat starts with a tiny electrical impulse near the top of the heart which spreads through the heart muscle and makes it squeeze (contract).
The electrical impulse travels first through the walls of the atria, which contract to pump blood into the ventricles. The impulse then travels through to walls of the ventricles, which contract to pump blood into the arteries.
What is heart failure?
In a normal healthy heart, during each heartbeat a set amount of blood enters the heart and is pumped out again. If you have heart failure, your heart cannot cope with pumping the full amount of blood in each heartbeat.
Heart failure is usually classified on which heart function or which side of the heart is most affected, rather than the actual cause of your heart failure.
The main types are:
- Systolic heart failure:
This means that the ventricles of the heart do not contract properly during each heartbeat, so blood is not adequately pumped out of the heart. In some cases, there is only a slight reduction in the power of the ventricle, which causes mild symptoms. If the power of the pumping action is more reduced, then symptoms become more severe. - Diastolic heart failure:
This occurs when the ventricle does not fill up with blood enough when the heart rests in between each heartbeat. This can sometimes be due to the wall of the ventricle being stiffer than usual. This makes it more difficult to stretch. - A combination of the above two types:
Heart failure may affect only the right ventricle (right-sided heart failure) or the left ventricle (left-sided heart failure), or both.
How common is heart failure?
There are around 68,000 new cases of heart failure diagnosed in the UK each year. Heart failure becomes more common as people become older. About 1 in 15 of people aged 75-84 and just over 1 in 7 people aged 85 and above have heart failure. It is uncommon in younger people.
Causes
What causes heart failure?
Heart failure is not an exact term. Heart failure is a general umbrella term and may develop as a complication of various conditions. Conditions that cause heart failure affect the ability of the heart to function well as a pump.
Conditions that may cause heart failure include the following:
Coronary heart disease (CHD):
CHD is the most common cause of heart failure. In this condition, the blood flow to the heart muscle is reduced by narrowing of the coronary arteries that supply the heart muscle with blood and oxygen - eg, as a result of atheroma. (Atheroma are small fatty lumps which develop within the inside lining of arteries.) The heart muscle may then not function as well as normal. Other symptoms of CHD may occur, such as having heart pains (angina). CHD is common in the UK and heart failure is a complication that occurs in some cases.
In particular, heart failure may develop after a heart attack (myocardial infarction). A heart attack is a complication of CHD and causes part of the heart muscle to die. Scar tissue forms in the affected part of the heart muscle. The larger the heart attack (and area of scar tissue), the more the function of the heart is affected.
Other causes:
Various other conditions can also cause heart failure - for example:
- Diseases of the heart muscle (cardiomyopathy).
- High blood pressure (hypertension).
- Diseases of the heart valves.
- Some types of abnormal heart rhythms (arrhythmias).
- Medicines and other chemicals that may damage the heart muscle - for example, alcohol excess, cocaine and some types of chemotherapy.
- Various non-heart conditions that can affect the function of the heart - for example, severe anaemia, thyroid disease (hypothyroidism or hyperthyroidism) and Paget's disease of bone.
Sometimes the cause of heart failure is not known.
Symptoms
What are the symptoms of heart failure?
The symptoms that may develop depend upon the type of heart failure that you have. Generally, left heart failure causes you to be short of breath (breathlessness). This is generally worse when you exert yourself (for example, walking up hill) or when you are lying flat in bed. This shortness of breath can be associated with a cough.
The main symptom of right heart failure is swollen ankles and legs. This is due to the build-up of excess fluid in your legs. Your liver may also become enlarged.
Other symptoms of heart failure (on either side of the heart) can include:
- Tiredness
- Dizziness
- Feeling sick
- Constipation
- Loss of appetite
Depending on the underlying cause for the heart failure, you may also have other symptoms. For example, chest pains if you have angina, the sensation of having a 'thumping heart' (palpitations) if you have a heart rhythm problem, etc.
The severity of heart failure is often graded into four classes:
- Class 1 (very mild): ordinary physical activity does not cause breathlessness, extreme tiredness (fatigue), or palpitations. You may not have any symptoms at all. However, tests (perhaps done for other reasons) may have detected mild heart failure.
- Class 2 (mild): you are comfortable at rest. However, ordinary physical activity such as walking causes some breathlessness, fatigue, or palpitations.
- Class 3 (moderate): although comfortable at rest, slight physical activity such as dressing yourself causes breathlessness, fatigue, or palpitations.
- Class 4 (severe): you are unable to carry out any physical activity without developing breathlessness, fatigue, or palpitations. Symptoms are often present even at rest. With any physical activity you have increased symptoms and discomfort.
Diagnosis
How is heart failure diagnosed?
When a doctor examines you, he or she may find signs that occur with heart failure - for example:
- An enlarged heart.
- A faster than normal pulse.
- Signs of fluid retention (such as swollen ankles, an enlarged liver or crackles in the lungs when the chest is examined).
However, these signs and the symptoms mentioned above can be due to various conditions other than heart failure. Therefore, if heart failure is suspected, tests are usually done to confirm the diagnosis.
If your own doctor suspects that you may have heart failure, then you are likely to be referred to a specialist heart failure clinic at a hospital.
Tests that are usually done include a 'heart tracing' (electrocardiogram, or ECG). Also, an ultrasound scan of the heart (echocardiogram) may be done. This painless test can usually confirm the presence of heart failure and can often diagnose the cause of the heart failure. A blood test to check for a substance called natriuretic peptide may be done in some cases, as this tends to be raised in people with heart failure. Other tests such as a chest X-ray, a urine test or other blood tests may also be advised to rule out other causes of the symptoms.
What can I do to help?
- Diet: If you are overweight, try to lose weight to reduce the extra burden on your heart. Do not have too much salt in your diet, as salt can cause water retention. For example, do not add salt to your food at the table and avoid cooking with it.
- Do not smoke: The chemicals in tobacco cause blood vessels to narrow, which can make heart failure worse. Smoking can also make CHD worse. You may benefit from being referred to a local 'stop smoking' clinic if you are finding it hard to stop smoking.
- Exercise: For most people with heart failure, regular exercise is advised. The fitter the heart, the better it will pump. The level of exercise to aim for will vary from person to person. Before you start to increase your exercise, get the go-ahead from your doctor, as some people with heart valve problems should not exercise. If you are not used to exercise, you could start by going for a daily walk.
- Immunisation: You should have an annual influenza jab and be immunised against the pneumococcal germ (bacterium).
- Weigh yourself each morning if you have moderate-to-severe heart failure. If you retain fluid rapidly, your weight goes up rapidly too. So, if your weight goes up by more than 2 kg (about 4 lb) over 1-3 days, you should contact a doctor. You may need an increase in your medication.
- Alcohol: You should not exceed the recommended amount of alcohol, as more than the recommended upper limits can be harmful.
Treatment
What medicines are used to treat heart failure?
The following medications are commonly used to treat heart failure. They will be tailored to the individual person, depending on the cause and severity of the heart failure.
Angiotensin-converting enzyme (ACE) inhibitors:
Most people with heart failure are prescribed an ACE inhibitor. There are several types and brands. These medicines prevent a build-up of fluid by interfering with a body chemical (the enzyme called angiotensin) which is involved in regulating body fluid. ACE inhibitors also have a protective effect on the heart and may slow down the progression of heart failure.
Some points to note about ACE inhibitors are below:
- After the very first dose, on the first day you start an ACE inhibitor:
- Stay indoors for about four hours, as occasionally some people feel dizzy. This is because the very first dose causes a drop in blood pressure in a few people.
- If you do feel dizzy, sit or lie down and it will usually ease off.
- If you become very dizzy, contact your doctor immediately.
- Your body quickly becomes used to the new medicine. After the first dose on the first day of treatment, there is no need to take any special precautions.
- A low dose is usually started at first but built up to a standard dose over 2-4 weeks.
- A blood test is usually done before starting an ACE inhibitor and again about 7-10 days after the first dose. This checks the function of your kidneys. The kidneys are affected in a very small number of people who take an ACE inhibitor. A blood test is then taken at regular intervals.
Angiotensin-II receptor antagonists:
These work in a similar way to ACE inhibitors. One may be used instead of an ACE inhibitor if you have problems or side-effects with taking an ACE inhibitor (such as a persistent cough).
Beta-blockers:
A beta-blocker medicine such as bisoprolol or carvedilol is usually prescribed in addition to an ACE inhibitor. Like ACE inhibitors, beta-blockers have a protective effect on the heart. A low dose is started at first and then increased every few weeks until a regular dose is reached. Occasionally, beta-blockers cause an initial worsening of symptoms before symptoms improve.
Research studies have shown that ACE inhibitors and beta-blockers not only help to ease symptoms but can improve the outlook and extend life expectancy for people with heart failure. Therefore, even if your symptoms go, you should continue to take these medicines if they are prescribed.
Diuretics ('water tablets'):
A diuretic is commonly needed to ease fluid retention. This is taken in addition to an ACE inhibitor and beta-blocker. Diuretics work on the kidneys and make you pass out extra urine. This helps to clear excess body fluid that builds up. There are different types and brands of diuretics. The dose depends on how bad your fluid retention has become and can be increased if necessary if your fluid retention becomes worse.
Diuretic medicines are normally taken in the morning. This is so the extra toilet trips are during the day and not at night. (Their effect on making extra urine lasts about six hours.) However, they can be taken at other times. For example, if you plan a morning shopping trip, take the diuretic tablet when you return.
Mineralocorticoid/aldosterone receptor antagonists (MRAs):
These medicines, such as spironolactone and eplerenone, also prevent the build-up of fluid. They interfere with the enzyme angiotensin which is involved in regulating body fluid. Research has shown that they improve your outlook. They may reduce your risk of needing to be in hospital and may extend your life expectancy.
Angiotensin is produced in your kidneys. If your kidney function is not good, you may not be able to take these medicines. Regular blood tests are used to monitor how your kidneys are coping.
1 in 10 men who take spironolactone may also have breast tenderness and enlargement.
Other medications:
Newer medicines are being developed and tested constantly. They may not be widely available. Ivabradine can be used for people with moderate or severe heart failure. Research has shown that people taking ivabradine have a reduced risk of worsening heart failure, hospital admission and death compared with those who did not take it. One of the main effects of ivabradine is to reduce the heart rate, which may have a protective effect on the heart.
Aspirin may be advised for people who have had a heart attack in the past.
Anticoagulants may be advised for those who have had a clot in the past. Your doctor will be able to give you more information if you need additional medications.
Note: it is very important that you take the tablets that have been prescribed for you. You should discuss with your doctor if you stop taking any of your tablets.
Devices for heart failure
Various devices are implanted in a small number of people with heart failure who have reduced function of their left ventricles. Examples include implantable cardioverter defibrillators (ICDs) and pacemakers.
ICDs work by detecting any abnormal heart rhythms that may occur. If your heart rhythm is too slow, the device can give your heart extra support by working as a normal pacemaker. If your heart beats too fast, the ICD can give you a burst of extra beats at a slightly faster rate which should return your heart back to a normal rhythm, or it can give you a shock (defibrillation) to restore a regular heartbeat.
Pacemakers work differently. In some cases, there is some damage to the specialised heart cells that carry the signals needed for your heart to squeeze (contract) properly. This can then cause the signals to travel out of synch which leads to your heart pumping less forcefully and less efficiently. The pacemakers work to control these signals, so the heart can then beat more effectively. This is also known as cardiac resynchronisation therapy.
These different devices have dramatically altered the treatment of heart failure in selected cases and have improved both the outlook and quality of life. However, these devices are only suitable for certain people with heart failure. Your doctor will be able to discuss with you in more detail if you are suitable for one of these devices.
Other treatments
As mentioned above, heart failure usually develops as a complication of various conditions. Other treatments for the underlying condition may be advised in certain cases.
For example:
- Treatment to lower blood pressure if you have high blood pressure (hypertension).
- Treatments to slow down the progression of CHD if this is the cause of the heart failure. For example, lowering a high cholesterol level.
- Surgery to replace or fix a heart valve may be done if a damaged heart valve is the cause of the heart failure.
- A heart transplant is an option in some cases.
Prognosis
What is the outlook (prognosis)?
It is difficult to give an outlook for an individual. In general, the more severe the heart failure, the worse the outlook. In many cases, the symptoms remain at a stable level for quite some time (months or years) before becoming worse. In some cases, the severity and symptoms become gradually worse over time.
Over a period of 15 years or so, various new treatments have been introduced which have led to a much-improved outlook for people with heart failure.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).