Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Osteoporosis
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the Cleveland Clinic, Ohio. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is osteoporosis?
Osteoporosis ("porous bone") is a disease that weakens bones, putting them at greater risk for sudden and unexpected fractures. Osteoporosis results in an increased loss of bone mass and strength. The disease often develops without any symptoms or pain, and it is usually not discovered until the weakened bones cause painful fractures. Most of these are fractures of the hip, wrist, and spine.
Although osteoporosis occurs in both men and women, women are four times more likely to develop the disease than men. After age 50, one in two white women, and one in four white men, will have an osteoporosis-related fracture in their lifetimes. Another 30 percent have low bone density that puts them at risk of developing osteoporosis (including African-Americans).
There are steps you can take to prevent osteoporosis from ever occurring. Treatments can also slow the rate of bone loss if you do have osteoporosis.
Who is at risk for developing osteoporosis?
There are many risk factors that increase your chance of developing osteoporosis:
- Gender: Women over the age of 50 or postmenopausal women have the greatest risk of developing osteoporosis. Women undergo rapid bone loss in the first 10 years after entering menopause, because menopause slows the production of estrogen, a hormone that protects against excessive bone loss.
- Age: Your risk for osteoporosis fractures increases as you age.
- Race: Caucasian and Asian women are more likely to develop osteoporosis. However, African-American and Hispanic women are still at risk. In fact, African-American women are more likely than white women to die after a hip fracture.
- Bone structure and body weight: Petite and thin people have a greater risk of developing osteoporosis because they have less bone to lose than people with more body weight and larger frames.
- Family history: If your parents or grandparents have had any signs of osteoporosis, such as a fractured hip after a minor fall, you may have a greater risk of developing the disease.
- Nutrition: You are more likely to develop osteoporosis if your body doesn't have enough calcium and vitamin D.
- Lifestyle: People who lead sedentary (inactive) lifestyles have a higher risk of osteoporosis.
- Medications: Certain medications cause side effects that may damage bone and lead to osteoporosis. These include steroids, treatments for breast cancer, and medications for treating seizures.
- Smoking: Smoking increases the risk of fractures.
- Alcohol use: Having one to two drinks a day (or more) increases the risk of osteoporosis.
- Medical conditions: People who have had the following should consider earlier screening for osteoporosis (this is not a complete list): Overactive thyroid, parathyroid, or adrenal glands, history of bariatric (weight loss) surgery, hormone treatment for breast or prostate cancer, eating disorders (bulimia, anorexia)
Causes
What causes osteoporosis?
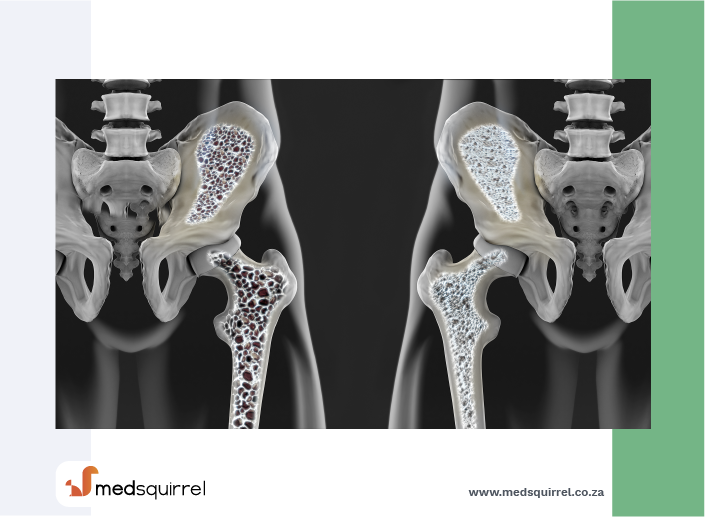
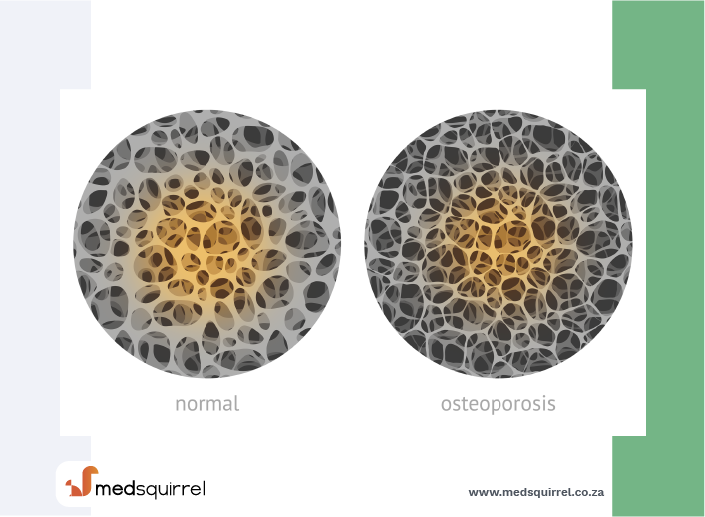
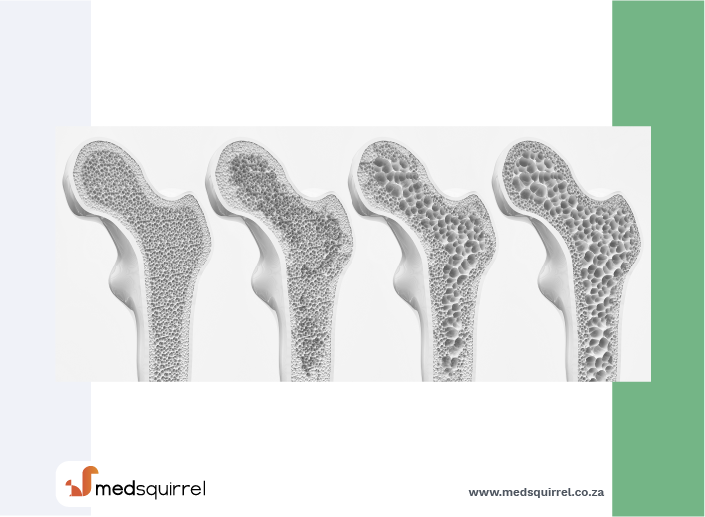
Though the exact cause of osteoporosis is unknown, we do understand how the disease develops. Your bones are made of living, growing tissue. The inside of healthy bone looks like a sponge; this area is called trabecular bone. An outer shell of dense bone wraps around the trabecular, or spongy bone. This hard shell is called cortical bone. When osteoporosis occurs, the "holes" in the "sponge" grow larger and more numerous, which weakens the inside of the bone.
In addition to supporting the body and protecting vital organs, bones store calcium and other minerals. When the body needs calcium, it breaks down and rebuilds bone. This process, called "bone remodeling," supplies the body with needed calcium while keeping the bones strong.
Up until about age 30, a person normally builds more bone than he or she loses. After age 35, bone breakdown occurs faster than bone buildup, which causes a gradual loss of bone mass. A person who has osteoporosis loses bone mass at a greater rate. After menopause, the rate of bone breakdown occurs even more quickly.
Diagnosis
How can I know if I have osteoporosis?
Painless and accurate medical tests can give you information about your bone health before problems begin.
Bone mineral density (BMD) tests, or bone measurements, also known as dual X-ray absorptiometry (DXA) scans, are X-rays that use very small amounts of radiation to determine the bone density of the spine, hip, or wrist.
Your physician can order these tests for you. All women over the age of 65 should have a bone density test. The DXA scan is done earlier for women who have risk factors for osteoporosis.
Men over age 70, or younger men with risk factors, should also consider getting a bone density test.
Treatment
When should osteoporosis be treated with medication?
Women whose bone density test shows T-scores of -2.5 or lower should begin therapy to reduce their risk of fracture. Many women need treatment if they have osteopenia, which is bone weakness that is not as severe as osteoporosis.
Your doctor might use the World Health Organization fracture risk assessment tool, or FRAX, to see if you qualify for treatment based on your risk factors and bone density results.
People who have had a typical osteoporosis fracture, such as that of the wrist, spine, or hip, should also be treated (sometimes even if the bone density results are normal).
How is osteoporosis treated?
Treatments for established osteoporosis include:
- Weight-bearing exercise
- Calcium and vitamin D supplements
- Medications:
- Estrogen therapy (women only)
- Bisphosphonates: i.e. aledronate sodium, risedronate, ibandronate, zoledronic acid
- Selective estrogen receptor modulators: raloxifene (women only)
- Strontium ranelate
- Parathyroid hormone: teriparatide
- Biologic therapy: denosumab
- Your doctor will select the most appropriate therapy.
Prevention
How can I prevent osteoporosis?
Your diet and lifestyle are two important risk factors you can control to prevent osteoporosis. Replacing lost estrogen with hormone therapy also provides a strong defense against osteoporosis in postmenopausal women.
Diet
To maintain strong, healthy bones, you need a diet rich in calcium throughout your life. One cup of milk contains 300 milligrams of calcium. Besides dairy products, other good sources of calcium are salmon with bones, sardines, kale, broccoli, calcium-fortified juices and breads, dried figs, and calcium supplements.
It is best to try to get the calcium from food and drink. For those who need supplements, remember that the body can only absorb 500 mg of calcium at a time. You should take your calcium supplements in divided doses, since anything more than 500 mg will not be absorbed.
Vitamin D is also important because it enables the body to absorb calcium. The recommended daily allowances of vitamin D are listed below. Vitamin D can also be obtained from sunlight exposure a few times a week or by drinking fortified milk.
Please ask your doctor for more detailed information about getting the right amount of calcium and vitamin D. In some cases, your doctor might recommend higher doses of vitamin D.
Lifestyle
Maintaining a healthy lifestyle can reduce the degree of bone loss. Begin a regular exercise program, and don't use too much alcohol and tobacco. Exercises that make your muscles work against gravity (such as walking, jogging, aerobics, and weightlifting) are best for strengthening bones.
Recommended websites
For further reading go to:
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).