Procedures Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription platform or service. Always refer any concerns or questions about diagnosis, treatment or prescription to your doctor.
Exercise Electrocardiogram (ECG/EKG)
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Healthwise, authored by Healthwise Staff (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is an exercise electrocardiogram (EKG/ECG)?
An exercise electrocardiogram (EKG or ECG) is a test that checks for changes in your heart while you exercise. Sometimes EKG abnormalities can be seen only during exercise or while symptoms are present. This test is sometimes called a "stress test" or a "treadmill test." During an exercise EKG, you may either walk on a motor-driven treadmill or pedal a stationary bicycle.
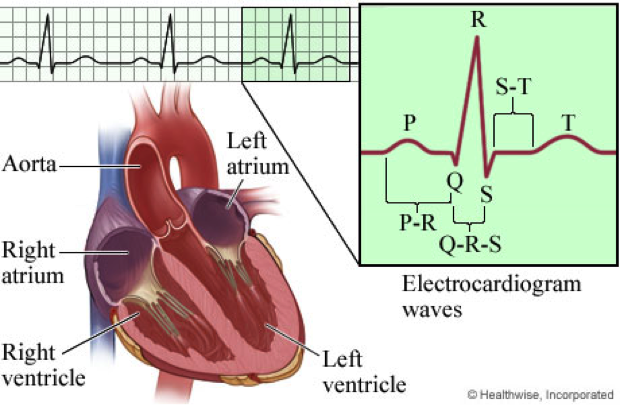
The heart is a muscular pump made up of four chambers. The two upper chambers are called atria, and the two lower chambers are called ventricles. A natural electrical system causes the heart muscle to contract and pump blood through the heart to the lungs and the rest of the body.
An exercise EKG translates the heart's electrical activity into line tracings on paper. The spikes and dips in the line tracings are called waves.
A resting EKG is always done before an exercise EKG test, and results of the resting EKG are compared to the results of the exercise EKG. A resting EKG may also show a heart problem that would make an exercise EKG unsafe.
Chambers of the heart
The heart has four chambers: two atria and two ventricles.
- The right atrium receives oxygen-poor blood from the body and pumps it to the right ventricle.
- The right ventricle pumps the oxygen-poor blood to the lungs.
- The left atrium receives oxygen-rich blood from the lungs and pumps it to the left ventricle.
- The left ventricle pumps the oxygen-rich blood to the body.

The Heart and its Electrical System
The heart has four chambers. The two upper chambers are called atria (the right atrium and the left atrium), and the two lower chambers are called ventricles.
Normally, the heartbeat starts in the right atrium in a group of special heart cells called the sinoatrial (or sinus) node. These cells act as a pacemaker for the heart.
The heart's pacemaker sends out an electrical signal (impulse) that spreads throughout the heart along electrical pathways. These pathways transmit the signal from the upper to the lower chambers of the heart, which causes the heart muscle to contract. Regular, rhythmic electrical signals keep the heart pumping blood to the lungs and the body.

Electrocardiogram (EKG/ECG) Components and Intervals
An electrocardiogram (EKG, ECG) is a test that measures the electrical signals that control heart rhythm. The test measures how electrical impulses move through the heart muscle as it contracts and relaxes.
The electrocardiogram translates the heart's electrical activity into line tracings on paper. The spikes and dips in the line tracings are called waves.
- The P wave is a record of the electrical activity through the upper heart chambers (atria).
- The QRS complex is a record of the movement of electrical impulses through the lower heart chambers (ventricles).
- The ST segment shows when the ventricle is contracting but no electricity is flowing through it. The ST segment usually appears as a straight, level line between the QRS complex and the T wave.
- The T wave shows when the lower heart chambers are resetting electrically and preparing for their next muscle contraction.
Why an EKG/ECG is done
An exercise electrocardiogram is done to:
- Help find the cause of unexplained chest pain or pressure.
- Help decide on the best treatment for a person with angina.
- See how well people who have had a heart attack or heart surgery are able to tolerate exercise.
- Help find the cause of symptoms that occur during exercise or activity, such as dizziness, fainting, or rapid, irregular heartbeats (palpitations).
- Check for a blockage or narrowing of an artery after a medical procedure, such as angioplasty or coronary artery bypass surgery, especially if the person has chest pain or other symptoms.
- See how well medicine or other treatment for angina or an irregular heartbeat is working.
- Help you make decisions about starting an exercise program if you have been inactive for a number of years and have an increased chance of having heart disease.
Exercise electrocardiograms are not recommended if you're healthy and have no symptoms of heart disease.
How to prepare for an EKG/ECG
Tell your doctor if you:
- Are taking any medicines, including a medicine for an erection problem (such as Viagra). You may need to take nitroglycerin during this test, which can cause a serious reaction if you have taken a medicine for an erection problem within the previous 48 hours. Ask your doctor whether you need to stop taking any of your other medicines before the test.
- Are allergic to any medicines, such as those used to numb the skin (anaesthetics).
- Take a blood thinner, or if you have had bleeding problems.
- Have joint problems in your hips or legs that may make it hard for you to exercise.
- Are or might be pregnant.
Your doctor may recommend how you should eat before the test. For example, your doctor may suggest you only eat a light breakfast before your test.
An exercise EKG may be dangerous and should not be done in some situations.
Be sure to tell your doctor if you:
- Think you are having a heart attack.
- Are having angina that is not relieved with rest (unstable angina).
- Have high blood pressure that is not controlled with medicine.
- Have untreated, life-threatening irregular heart rhythms (arrhythmias).
- Have severe narrowing of one of your heart valves (aortic valve stenosis).
- Have inflammation in your heart muscle (myocarditis).
- Have a severe decrease in the amount of red blood cells (anaemia).
- Have a stretched and bulging section in the wall of the large artery that carries blood from the heart (aortic aneurysm) or in one of the chambers of the heart (ventricular aneurysm).
- Have severe lung disease.
Remove all jewellery from your neck, arms, and wrists. Wear flat, comfortable shoes (no bedroom slippers) and loose, lightweight shorts or sweat pants. Men are usually bare-chested during the test. Women often wear a bra, T-shirt, or hospital gown. Avoid wearing any restrictive clothing other than a bra.
You may want to stretch your arm and leg muscles before beginning an exercise EKG.
How an EKG/ECG is done
An exercise electrocardiogram (EKG or ECG) is usually done in a doctor's office, clinic, or hospital lab by a health professional or doctor. An internist, family medicine doctor, or cardiologist evaluates the test results.
Before the test
Areas on your arms, legs, and chest where small pads or patches (electrodes) will be placed are cleaned and may be shaved to provide a clean, smooth surface to attach the electrodes.
The electrodes are hooked to a machine that traces your heart activity onto a piece of paper. Your chest may be loosely wrapped with an elastic band to keep the electrodes from falling off during exercise. A blood pressure cuff will be wrapped around your upper arm so that your blood pressure can be checked every few minutes during the test.
During the test
For exercise, you typically either walk on a treadmill or pedal on a stationary bicycle while being monitored by an EKG machine. Your EKG will be monitored on screen, and paper copies will be printed out for later review before you start the exercise, at the end of each section of exercise, and while you are recovering.
The test is usually performed in a series of stages, each lasting 3 minutes. After each 3-minute stage, the resistance or speed of the treadmill or bicycle is increased.
For the treadmill test, the treadmill will move slowly in a level or slightly inclined position. As the test progresses, the speed and steepness of the treadmill will be increased so that you will be walking faster and at a greater incline.
For the stationary bicycle, you will sit on the bicycle with the seat and handlebars adjusted so that you can pedal comfortably. You can use the handlebars to help you balance, but you should not use them to support your weight. You will be asked to pedal fast enough to maintain a certain speed. The resistance will then be gradually increased, making it harder to pedal.
In both the treadmill and the bicycle tests, your EKG, heart rate, and blood pressure will be recorded during the exercise. Your heart rate and EKG will be recorded continuously. Your blood pressure is usually measured during the second minute of each stage. It may be measured more frequently if the readings are too high or too low. During the test, you might be asked to give a number that answers the question "How hard do you feel the exercise is?" The number will be on a scale from 6 to 20 and is called a rating of perceived exertion.
The test continues until you need to stop, until you reach your maximum heart rate, until you begin to show symptoms of stress on your heart and lungs (such as fatigue, extreme shortness of breath, or angina), or until the EKG tracing shows decreased blood flow to your heart muscle.
The test may also be stopped if you develop serious irregular heartbeats or if your blood pressure drops below your resting level.
After the test
When the exercise phase is completed:
- You will be able to sit or lie down and rest.
- Your EKG and blood pressure will be checked for about 5 to 10 minutes during this time.
- The electrodes are then removed from your chest, and you may resume your normal activities.
Do not take a hot bath or shower for at least an hour, since hot water after vigorous exercise can make you feel dizzy and faint.
The entire test usually takes 15 to 30 minutes.
How an EKG/ECG Feels
The electrodes may feel cool when they are put on your chest. If you have a lot of hair on your chest, a small area under each electrode may need to be shaved. When the electrodes are taken off, they may pull your skin a little.
The room where the exercise electrocardiogram is done may be kept cool for comfort, since you will warm up rapidly when you begin to exercise.
The blood pressure cuff on your arm will be inflated every few minutes. This will squeeze your arm and feel tight. Tell your health professional if this is painful.
While exercising, you may have leg cramps or soreness; feel tired, short of breath, or lightheaded; have a dry mouth; and sweat. You might even have some mild chest pain or pressure. Tell the health professional or doctor if you have these symptoms.
Risks
An exercise electrocardiogram is generally safe. Emergency equipment will be available in the testing area.
Risks include:
- Irregular heartbeats during the test.
- Severe angina symptoms.
- Fainting.
- Falling.
- Heart attack.
The electrodes are used to transfer an image of the electrical activity of your heart to tracing on paper. No electricity passes through your body from the machine, and there is no danger of getting an electrical shock.
EKG/ECG Results
An exercise electrocardiogram (EKG or ECG) is a test that checks for changes in your heart while you exercise. Your doctor may be able to talk to you about your results right after the test. But complete test results may take several days.
Your doctor will look at the pattern of spikes and dips on your electrocardiogram to check the electrical activity in different parts of your heart. The spikes and dips are grouped into different sections that show how your heart is working.
Normal EKG/ECG results
- You reach your target heart rate (based on your age) and can exercise without chest pain or other symptoms of heart disease
- Your blood pressure increases steadily during exercise.
- Your EKG tracings do not show any significant changes. Your heartbeats look normal.
Abnormal EKG/ECG results
- You have angina symptoms, such as chest pain or pressure, during or right after the test.
- You have other symptoms of heart disease, such as dizziness, fainting, or extreme shortness of breath.
- Your blood pressure drops or does not rise during exercise.
- The EKG tracing does not look normal.
- Your heartbeats are too fast, too slow, or very irregular.
Some people who have a normal exercise electrocardiogram test may still have heart disease, and some people with an abnormal test do not have heart disease.
What Affects the Test
You may not be able to have the test or the results may not be accurate if:
- The electrodes are not securely attached to the skin.
- You are not able to exercise hard enough during the test.
- You take certain medicines, such as digoxin, phenothiazines, and some antiarrhythmic medicines.
- You have a low potassium level.
- You smoke or eat a heavy meal before the test.
What To Think About
An exercise EKG is not always accurate. The test results from an exercise EKG are always evaluated along with other information, such as your symptoms and other risk factors.
The test is less accurate in young or middle-aged women who do not have typical symptoms of heart disease.
If your doctor recommends a test, ask what it is for and why you need it. You can help decide if a test is right for you. Talk with your doctor to make that decision.
Further tests, such as cardiac perfusion scanning, stress echocardiogram, or cardiac catheterization, may be needed to further evaluate an abnormal exercise EKG test result.
About the source
Healthwise Staff
Medical Reviewers:
- Rakesh K. Pai, MD, FACC - Cardiology, Electrophysiology
- Gregory Thompson, MD - Internal Medicine
- Martin J. Gabica, MD - Family Medicine
- Adam Husney, MD - Family Medicine
- George Philippides, MD – Cardiology
Current as of February 20, 2018
References
- S. Preventive Services Task Force (2012). Screening for coronary heart disease with electrocardiography: Recommendation statement. Available online: http://www.uspreventiveservicestaskforce.org/uspstf/uspsacad.htm.
- Chernecky CC, Berger BJ (2013). Laboratory Tests and Diagnostic Procedures, 6th ed. St. Louis: Saunders.
- Chou R, et al. (2011). Screening asymptomatic adults with resting or exercise electrocardiography: A review of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine, 155(6): 375–385.
- Fischbach F, Dunning MB III (2015). A Manual of Laboratory and Diagnostic Tests, 9th ed. Philadelphia: Wolters Kluwer Health.
- Gibbons RJ, et al. (2002). ACC/AHA 2002 guideline update for exercise testing: Summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation, 106(14): 1883–1892.
- Lauer M, et al. (2005). Exercise testing in asymptomatic adults. A statement for professionals from the American Heart Association Council on Clinical Cardiology, Subcommitee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation, 112(5): 771–776.
- Myers J, et al. (2009). Recommendations for clinical exercise laboratories. A scientific statement from the American Heart Association. Circulation, 119(24): 3144–3161.
- S. Preventive Services Task Force (2012). Screening for coronary heart disease with electrocardiography: Recommendation statement. Available online: http://www.uspreventiveservicestaskforce.org/uspstf/uspsacad.htm.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).