Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Hiatus Hernia
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Mary Harding (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Hiatus hernia is the term used to describe a condition where part of the stomach pushes up into the lower chest through a weakness in the diaphragm. The diaphragm is the large flat muscle that separates the lungs from the tummy (abdomen) and helps us to breathe. Not everyone with a hiatus hernia develops symptoms. However, if you have a hiatus hernia you are more prone to reflux acid into your gullet (oesophagus), which can cause heartburn and other symptoms. If symptoms do occur, treatment with acid-suppressing medication usually works well.
Understanding the upper gut
The gut (gastrointestinal tract) is the tube that starts at the mouth and ends at the back passage (anus).
The upper gut includes the gullet (oesophagus), stomach and the first part of the small intestine (the duodenum). Food passes down the oesophagus into the stomach. The stomach makes acid which is not essential but helps to digest food. After being mixed in the stomach, food passes into the duodenum to be digested.
The walls of the stomach contain muscle. At the junction of the stomach and the oesophagus there is a thickened area of muscle which is called a sphincter. The sphincter acts like a valve. When food comes down the oesophagus into the stomach, the sphincter relaxes. However, it closes at other times to stop food and acid in the stomach going back up (refluxing) into the oesophagus.
The diaphragm is a large flat muscle that separates the lungs from the tummy (abdomen). It helps us to breathe.
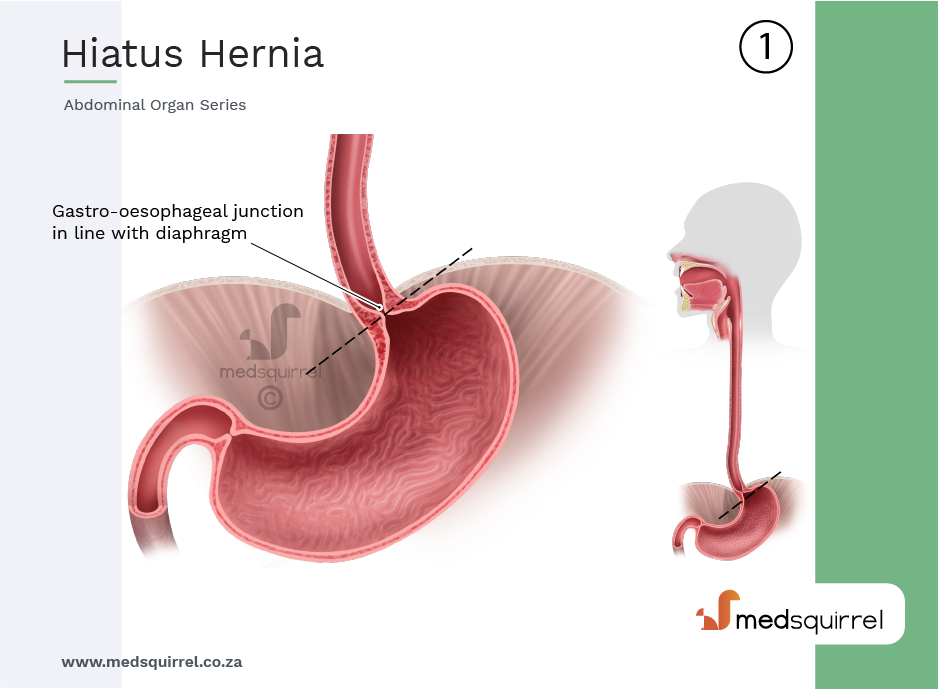
The oesophagus comes through a hole (hiatus) in the diaphragm just before it joins to the stomach. Normally, all of the stomach is below the diaphragm. The muscle fibres in the diaphragm around the lower oesophagus help the sphincter to keep the oesophagus closed to prevent reflux of acid and food.
What is a hernia and what is a hiatus hernia?
A hernia occurs when part of an organ pushes (protrudes) through a muscular wall that holds it in place. There are different types of hernia. For example, an inguinal hernia is the most common type when part of the lower bowel protrudes through the muscle in the groin.
A hiatus hernia occurs when part of one of the organs in the tummy protrudes through the diaphragm. Most commonly this is a part of the stomach; however, it may be other organs, such as the pancreas, spleen or the upper gut (small intestine).
Types of hiatus hernia
Sliding hiatus hernia is the most common type. In this situation, the sphincter muscle at the bottom of the gullet (oesophagus) and the top of the stomach protrudes through the hole (hiatus) in the diaphragm. This is the muscle separating the lungs from the tummy (abdomen). The hernia may slide up and down, in and out of the lower chest. It is often quite small. This type of hiatus hernia tends to be associated with symptoms of acid reflux (see below.)
Para-oesophageal hiatus hernia (also called a rolling hiatus hernia) is less common. In this situation, a part of the stomach pushes (protrudes) up through the hole in the diaphragm next to the oesophagus. Other organs from the tummy can also protrude through the hole in some cases. This could be the pancreas, the spleen or the upper gut (small intestine). This is not the normal type of hiatus hernia and it is much less common than a sliding hiatus hernia. It is more risky, as there is more chance the organ protruding can get stuck, causing a blockage (obstruction).


You may also see hiatus hernias referred to as types 1-4 depending on where the stomach and oesophagus are in relation to the diaphragm.
Causes
What causes hiatus hernia and how common is it?
The exact number of people with a hiatus hernia is not known, as many people with a hiatus hernia do not have symptoms. However, they are thought to be common. Some studies suggest that up to half of people having tests for indigestion (dyspepsia) are discovered to have a hiatus hernia.
The cause of hiatus hernia is not clear. It is thought that most develop in people over the age of 50 years. It may be that the diaphragm muscle weakens with age. This allows part of the stomach to protrude through the hole in the diaphragm. Factors which increase the pressure in the tummy (abdomen), such as regular coughing, repeated lifting of heavy objects, or obesity, may increase the risk of developing a hiatus hernia. It may be more likely if one of your close relatives has a hiatus hernia.
Operations around the stomach and gullet can make you more likely to get the para-oesophageal type of hiatus hernia. You are also more likely to get this type if your spine or rib cage is more curved than usual. For example, people with scoliosis or kyphosis.
There is a rare type of hiatus hernia which occurs in newborn babies, due to a congenital defect of the stomach or diaphragm. 'Congenital' means that the condition is present from birth. This rare type is not dealt with further in this leaflet.
Symptoms
What are the symptoms of hiatus hernia?
- Many people with a hiatus hernia have no symptoms.
- Others have acid reflux symptoms.
Acid Reflux Symptoms
The hernia itself does not cause symptoms. However, if you have a hiatus hernia, the factors that normally prevent stomach acid from refluxing into the gullet (oesophagus) may not work so well. The sphincter muscle may not work properly. The normal pressure of the diaphragm muscle on the oesophagus is lost. Therefore, you are more prone for acid in the stomach to go back upwards (reflux) into your oesophagus. The refluxed acid can cause inflammation of the lower part of the oesophagus.
This can cause one or more of the following symptoms:
- Heartburn: this is the main symptom. This is a burning feeling which rises from the upper tummy (abdomen) or lower chest up towards the neck. (It is confusing as it has nothing to do with the heart!)
- Pain in the upper abdomen and chest.
- Feeling sick.
- An acid taste in the mouth.
- Bloating.
- Belching.
- Difficulty swallowing.
- A burning pain when you swallow hot drinks.
These symptoms tend to come and go and tend to be worse after a meal.
Some uncommon symptoms may occur. If any of these symptoms occur, it can make the diagnosis difficult, as these symptoms can mimic other conditions. For example:
- A persistent cough, particularly at night, sometimes occurs. This is due to the refluxed acid irritating the windpipe (trachea). Asthma-like symptoms of cough and wheeze can sometimes be due to acid reflux.
- Other mouth and throat symptoms sometimes occur such as gum problems, bad breath, sore throat, hoarseness and a feeling of a lump in the throat.
- Severe chest pain develops in some cases (and may be mistaken for a heart attack).
- Rarely, in people with a para-oesophageal hernia, the symptoms can be those of a part of the bowel being blocked (obstructed). In this case there would be severe tummy pain or chest pain, with retching or being sick (vomiting).
Note: many people with acid reflux do not have a hiatus hernia. Also, many people with a hiatus hernia do not have symptoms of acid reflux. If you have a hiatus hernia it does not necessarily mean that the sphincter between the oesophagus and stomach does not work so well. It is just that having a hiatus hernia makes you more prone to having a poorly functioning sphincter and more prone to developing acid reflux symptoms.
However, people with a hiatus hernia who do get reflux, on average, tend to get more severe symptoms and problems associated with acid reflux. This may be because with a hiatus hernia any acid that gets into the oesophagus is more likely to remain in contact with the lining of the oesophagus for longer compared with people without a hiatus hernia.
Diagnosis
How is a hiatus hernia diagnosed?
A hiatus hernia may be diagnosed if you have tests for symptoms of reflux. A special X-ray test called a barium swallow is sometimes used to confirm the presence of a hiatus hernia. Endoscopy is increasingly being used for diagnosis. An endoscope is a thin, flexible telescope which is passed down the gullet (oesophagus) into the stomach. This allows a doctor or nurse to look inside. A hiatus hernia may be seen. Occasionally other tests are needed.
Treatment
What is the treatment of hiatus hernia?
No treatment in some cases
If you have no symptoms, in most cases you do not need any treatment. The hiatus hernia usually causes no harm. Occasionally, if you have a hernia which is at risk of complications, you may be offered surgery, even if you do not have any symptoms.
Lifestyle changes
- If you have reflux symptoms, you should aim to lose weight if you are overweight.
- Avoid anything that causes pressure on your stomach, such as tight clothing and corsets.
- If you are a smoker you should aim to stop. If you drink a lot of alcohol, it also helps to cut down on alcohol.
- Raising the head end of the bed may help with symptoms at night.
- Avoiding eating your dinner too close to bedtime may also help with symptoms at night. Aim to have your dinner at least three hours before you go to bed ideally.
- Smaller meals may be helpful, as may avoiding foods which you find make the reflux worse.
Medicines
If changing your lifestyle does not help, you may need medication. Medicines which reduce the action or production of stomach acid may help. The most effective medicines are proton pump inhibitors. Proton pump inhibitors often used are omeprazole or lansoprazole. If these do not suit you, other pills such as ranitidine or antacids may be used. You may need to take these for many years. Some people find they can take them as needed rather than every single day.
An operation
Rarely, a hiatus hernia causes severe symptoms of reflux which are not helped so well with medication. Therefore, an operation is occasionally advised. It may also be advisable if you cannot tolerate the medication for some reason. During this operation the stomach is put back into the correct position and the weakened diaphragm muscle around the lower gullet (oesophagus) is tightened. The operation is usually done these days using a laparoscope (a telescope inserted into the stomach). The operation quite often needs repeating in due course.
Complications
What are the possible complications of a hiatus hernia?
Possible complications may occur if you have long-term reflux of acid into the gullet (oesophagus), which occurs in some cases. These include:
- Oesophagitis: This is an inflammation of the lining of the gullet, caused by the acid washing against it over time. This can usually be treated with proton pump inhibitors as mentioned above.
- Cough: Sometimes the acid reflux can go back up and affect the voice box area (larynx) and give you a constant tickly cough. This can also usually be treated successfully with anti-reflux medicines.
- Narrowing (a stricture): If you have severe and long-standing inflammation it can cause scarring and narrowing of the lower oesophagus. This is uncommon.
- Twisting (volvulus) or strangulation (trapping of the hernia with blockage of the circulation): These are rare complications which can occur with the uncommon para-oesophageal type of hiatus hernia.
- Barrett's oesophagus: The lining of the oesophagus is made up of a number of units called cells. In Barrett's oesophagus the cells that line the lower oesophagus change. The changed cells are more prone than usual to becoming cancerous. (About 1 in 20 men and 1 in 33 women with Barrett's oesophagus develop cancer of the oesophagus.)
- Cancer: Your risk of developing cancer of the oesophagus is slightly increased compared with the normal risk if you have long-term acid reflux. This small increased risk is slightly higher still in people with reflux plus a hiatus hernia. This is because reflux problems, on average, tend to be more severe in people with a hiatus hernia compared to those without a hiatus hernia.
But note: it has to be stressed that most people with reflux or hiatus hernia do not develop any of these complications. They are uncommon. Tell your doctor if you have pain or difficulty when you swallow (food sticking), which may be the first symptom of a complication. See your doctor if your symptoms aren't being controlled by the medicines you have been prescribed, or if there is any change.
About the author
Dr Mary Harding
BA, MA, MB BChir, MRCGP, DFFP
Mary qualified at Cambridge in 1989. She joined EMIS as an author in 2013. Mary is a part-time, salaried GP at The Village Surgery, Wheathampstead and previously for 12 years in Welwyn Garden City. Mary is also an appraiser and Senior Appraiser for NHS England, in the Central Midlands area team.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).