Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Heartburn
Also known as Acid Reflux / Gastroesophageal Reflux Disease (GERD)

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the Mayo Clinic, Minnesota. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
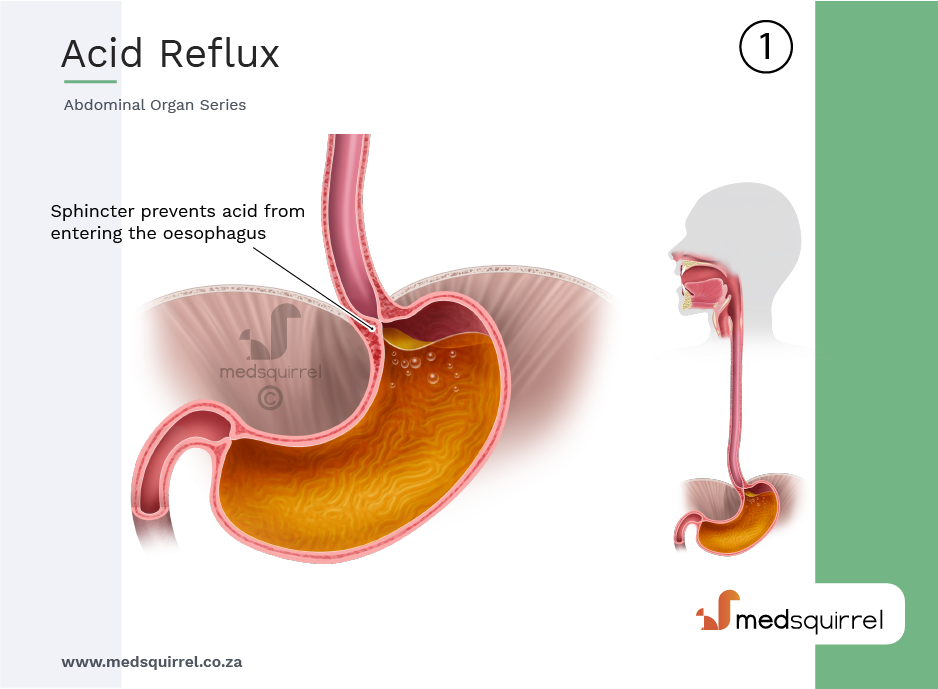
When you swallow, a circular band of muscle around the bottom of your oesophagus (lower oesophageal sphincter) relaxes to allow food and liquid to flow into your stomach. Then the sphincter closes again.
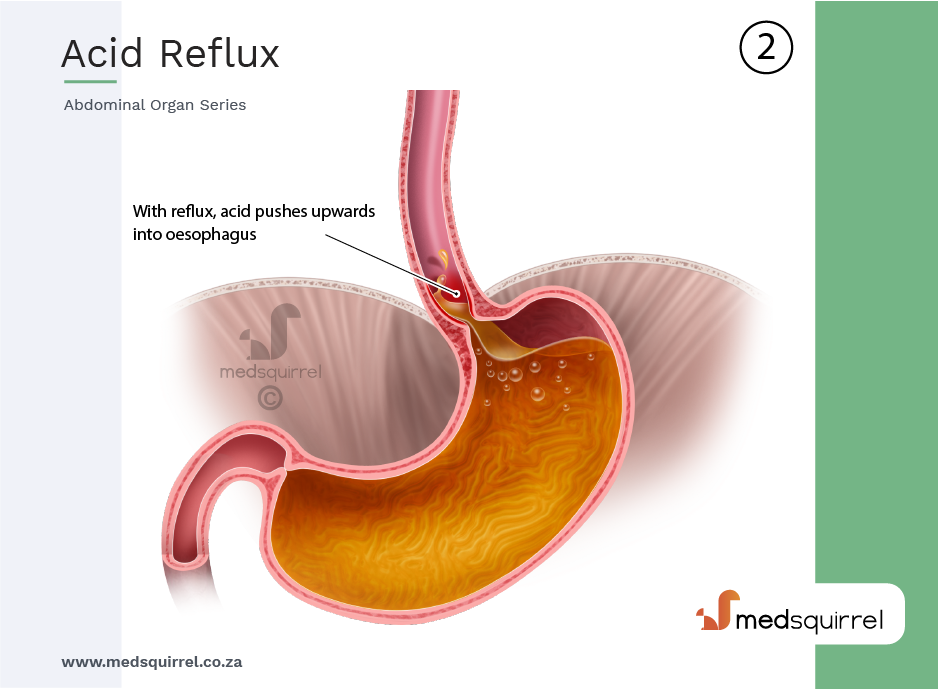
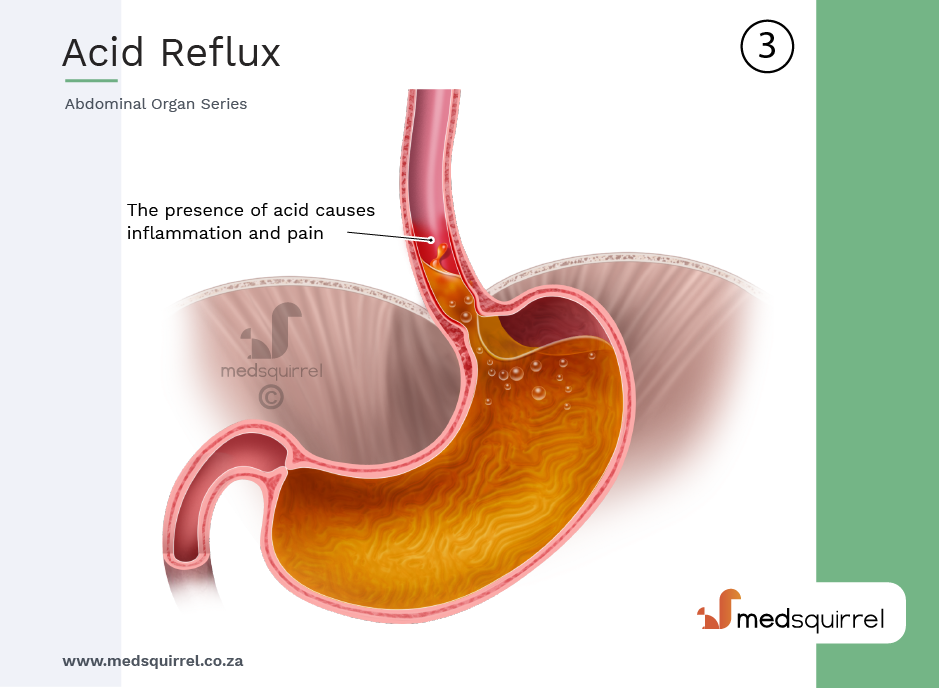
If the sphincter relaxes abnormally or weakens, stomach acid can flow back up into your oesophagus. This constant backwash of acid irritates the lining of your oesophagus, often causing it to become inflamed.
Gastroesophageal reflux disease (GERD) occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the lining of your oesophagus.
Many people experience acid reflux from time to time. GERD is mild acid reflux that occurs at least twice a week, or moderate to severe acid reflux that occurs at least once a week.
GERD is caused by frequent acid reflux.
How heartburn and GERD occur
Symptoms
Common signs and symptoms of GERD include:
- A burning sensation in your chest (heartburn), usually after eating, which might be worse at night
- Chest pain
- Difficulty swallowing
- Regurgitation of food or sour liquid
- Sensation of a lump in your throat
If you have night-time acid reflux, you might also experience:
- Chronic cough
- Laryngitis
- New or worsening asthma
- Disrupted sleep
When to see a doctor
Seek immediate medical care if you have chest pain, especially if you also have shortness of breath, or jaw or arm pain. These may be signs and symptoms of a heart attack.
Make an appointment with your doctor if you:
- Experience severe or frequent GERD symptoms
- Take over-the-counter medications for heartburn more than twice a week
Risk factors
Conditions that can increase your risk of GERD include:
- Obesity
- Bulging of the top of the stomach up into the diaphragm (hiatal hernia)
- Pregnancy
- Connective tissue disorders, such as scleroderma
- Delayed stomach emptying
Factors that can aggravate acid reflux include:
- Smoking
- Eating large meals or eating late at night
- Eating certain foods (triggers) such as fatty or fried foods
- Drinking certain beverages, such as alcohol or coffee
- Taking certain medications, such as aspirin
Complications
Over time, chronic inflammation in your oesophagus can cause:
Narrowing of the oesophagus (oesophageal stricture): Damage to the lower oesophagus from stomach acid causes scar tissue to form. The scar tissue narrows the food pathway, leading to problems with swallowing.
An open sore in the oesophagus (oesophageal ulcer): Stomach acid can wear away tissue in the oesophagus, causing an open sore to form. An oesophageal ulcer can bleed, cause pain and make swallowing difficult.
Precancerous changes to the oesophagus (Barrett's oesophagus): Damage from acid can cause changes in the tissue lining the lower oesophagus. These changes are associated with an increased risk of oesophageal cancer.
Diagnosis
Your doctor might be able to diagnose GERD based on a physical examination and history of your signs and symptoms.
To confirm a diagnosis of GERD, or to check for complications, your doctor might recommend:
Upper endoscopy / Gastroscopy:
Your doctor inserts a thin, flexible tube equipped with a light and camera (endoscope) down your throat, to examine the inside of your oesophagus and stomach. Test results can often be normal when reflux is present, but an endoscopy may detect inflammation of the oesophagus (esophagitis) or other complications. An endoscopy can also be used to collect a sample of tissue (biopsy) to be tested for complications such as Barrett's oesophagus.
X-ray of your upper digestive system:
X-rays are taken after you drink a chalky liquid that coats and fills the inside lining of your digestive tract. The coating allows your doctor to see a silhouette of your oesophagus, stomach and upper intestine. You may also be asked to swallow a barium pill that can help diagnose a narrowing of the oesophagus that may interfere with swallowing.
Ambulatory acid (pH) probe test:
A monitor is placed in your oesophagus to identify when, and for how long, stomach acid regurgitates there. The monitor connects to a small computer that you wear around your waist or with a strap over your shoulder. The monitor might be a thin, flexible tube (catheter) that's threaded through your nose into your oesophagus, or a clip that's placed in your oesophagus during an endoscopy and that gets passed into your stool after about two days.
Oesophageal manometry:
This test measures the rhythmic muscle contractions in your oesophagus when you swallow. Oesophageal manometry also measures the coordination and force exerted by the muscles of your oesophagus.
Treatment
Your doctor is likely to recommend that you first try lifestyle modifications and over-the-counter medications. If you don't experience relief within a few weeks, your doctor might recommend prescription medication or perhaps surgery.
Over-the-counter medications
The options include:
- Antacids that neutralize stomach acid: Antacids may provide quick relief. But antacids alone won't heal an inflamed oesophagus damaged by stomach acid. Overuse of some antacids can cause side effects, such as diarrhoea or sometimes kidney problems.
- Medications to reduce acid production: These medications — known as H-2-receptor blockers — include cimetidine, famotidine , nizatidine and ranitidine . H-2-receptor blockers don't act as quickly as antacids, but they provide longer relief and may decrease acid production from the stomach for up to 12 hours. Stronger versions are available by prescription.
- Medications that block acid production and heal the oesophagus: These medications — known as proton pump inhibitors — are stronger acid blockers than H-2-receptor blockers and allow time for damaged oesophageal tissue to heal. Over-the-counter proton pump inhibitors include lansoprazole and omeprazole.
Prescription medications
Prescription-strength treatments for GERD include:
- Prescription-strength H-2-receptor blockers: These include prescription-strength famotidine, nizatidine and ranitidine. These medications are generally well-tolerated but long-term use may be associated with a slight increase in risk of vitamin B-12 deficiency and bone fractures.
- Prescription-strength proton pump inhibitors: These include esomeprazole, lansoprazole, omeprazole, pantoprazole, rabeprazole and dexlansoprazole . Although generally well-tolerated, these medications might cause diarrhoea, headache, nausea and vitamin B-12 deficiency. Chronic use might increase the risk of hip fracture.
- Medication to strengthen the lower oesophageal sphincter: Baclofen may ease GERD by decreasing the frequency of relaxations of the lower oesophageal sphincter. Side effects might include fatigue or nausea.
Lifestyle and home remedies
Lifestyle changes may help reduce the frequency of acid reflux.
Try to:
- Maintain a healthy weight: Excess pounds put pressure on your abdomen, pushing up your stomach and causing acid to reflux into your oesophagus.
- Stop smoking: Smoking decreases the lower oesophageal sphincter's ability to function properly.
- Elevate the head of your bed: If you regularly experience heartburn while trying to sleep, place wood or cement blocks under the feet of your bed so that the head end is raised by 6 to 9 inches. If you can't elevate your bed, you can insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head with additional pillows isn't effective.
- Don't lie down after a meal: Wait at least three hours after eating before lying down or going to bed.
- Eat food slowly and chew thoroughly: Put down your fork after every bite and pick it up again once you have chewed and swallowed that bite.
- Avoid foods and drinks that trigger reflux: Common triggers include fatty or fried foods, tomato sauce, alcohol, chocolate, mint, garlic, onion, and caffeine.
- Avoid tight-fitting clothing: Clothes that fit tightly around your waist put pressure on your abdomen and the lower oesophageal sphincter
Surgery and other procedures
GERD can usually be controlled with medication.
If medications don't help or you wish to avoid long-term medication use, your doctor might recommend:
Fundoplication: The surgeon wraps the top of your stomach around the lower oesophageal sphincter, to tighten the muscle and prevent reflux. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. The wrapping of the top part of the stomach can be partial or complete.
LINX device: A ring of tiny magnetic beads is wrapped around the junction of the stomach and oesophagus. The magnetic attraction between the beads is strong enough to keep the junction closed to refluxing acid, but weak enough to allow food to pass through. The Linx device can be implanted using minimally invasive surgery.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).