First Aid Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
How to Perform the Heimlich Maneuver on a Toddler
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website wikiHow. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
It's common for toddlers to put items and food in their mouths. Sometimes, this tendency can cause a toddler to choke. Children can lose consciousness quickly so it's important to know how to effectively clear the airway by performing the Heimlich maneuver. If the Heimlich maneuver fails to dislodge the item obstructing the airway and the child becomes unconscious, you'll need to move on to CPR.
Part 1: Assessing the Situation
1. See if your toddler can speak
When someone is choking, they'll lose the ability to speak because air can't get through. Therefore, if you ask your toddler a question and she can't reply, she may be choking.
2. Look to see if the toddler is having trouble breathing
You may notice that he's having trouble drawing breaths. He may also be making weird noises when he's breathing, such as a high-pitched noise when drawing in a breath.
3. Look for weak coughing
Your toddler may be trying to cough up what's in her throat and failing. Therefore, the cough will be weak. A heavy cough likely indicates that enough air is getting through that she's not choking.
4. Check for blue tinges
Toddlers who aren't breathing may start turning blue around the edges. For instance, you may notice bluish or dusky tinges on her fingernails, lips, or skin.
- However, be aware that children and toddlers compensate much better than adults and may not turn blue as fast as an adult would.
5. Avoid intervening if the child is able to speak
If the child is able to speak or breathe well, don't start Heimlich. The same goes if the child is able to cough hard. However, be watching to make sure the symptoms don't suddenly worsen.
6. See if the toddler is conscious
Choking can cause a toddler to pass out. See if he can look at you when you talk by asking him a question. You'll likely need this information when you call 911. You'll also need to move on to the steps for an unconscious choking toddler if he's not conscious.
- You can also lightly flick the bottom of a toddler's foot to check for consciousness.
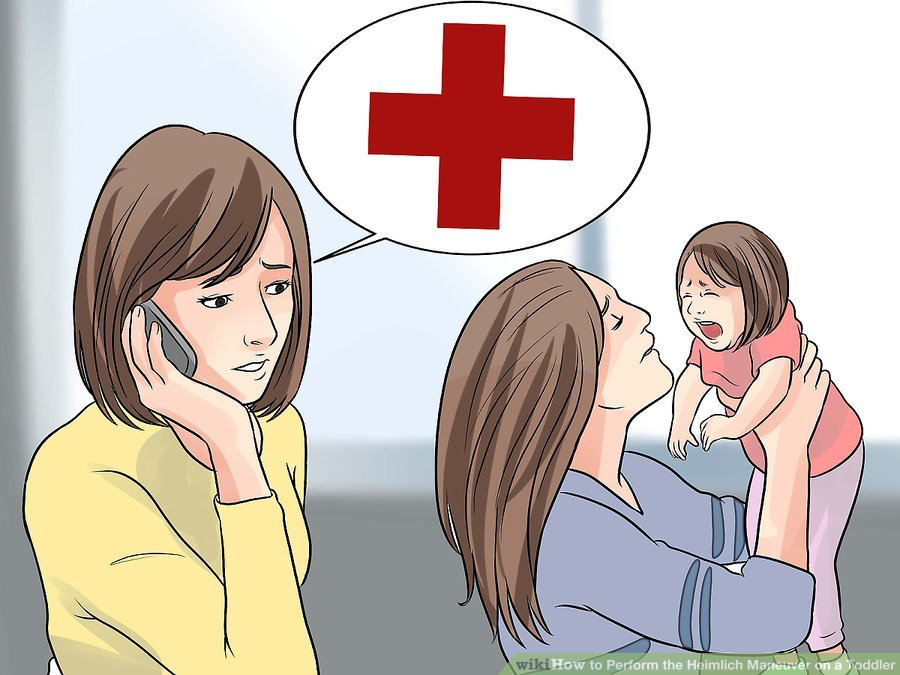
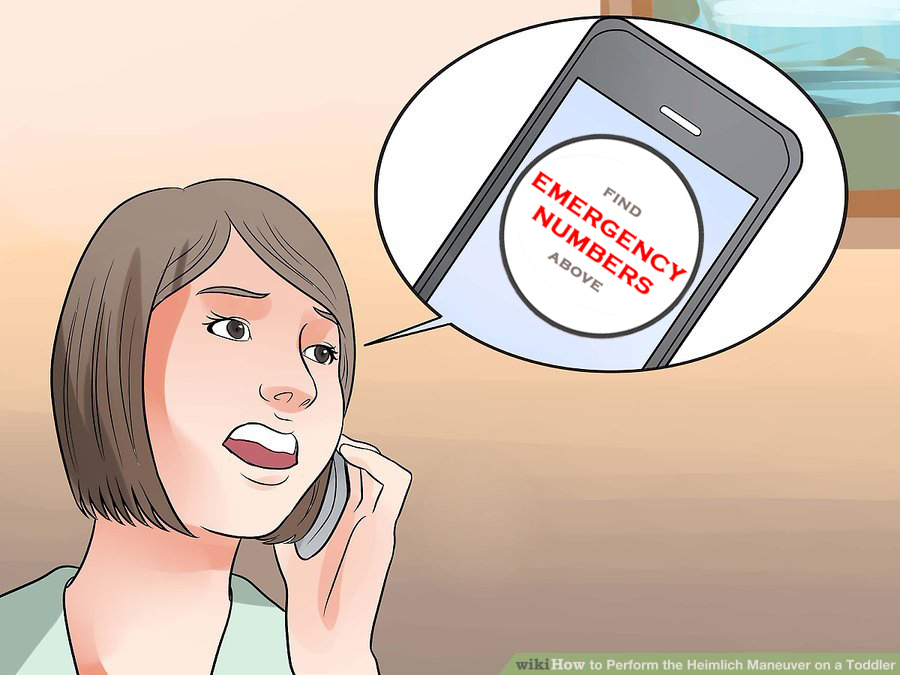
7. Ask someone to call emergency services (see "EMERGENCY NUMBERS" above)
If you are not alone with the child, ask someone to call emergency services (see "EMERGENCY NUMBERS" above). If you are, you should try the Heimlich maneuver before calling emergency services.
8. Ask for consent
If a parent is present, quickly ask for consent. Seconds count when saving a life. If a parent is not present, Good Samaritan laws in your state should cover any action you take in good faith to save the child's life.

Part 2: Performing the Heimlich Maneuver
1. Bend the child over
Have the child bend over at the waist. Place your hand under her chest for support.
- To perform this maneuver properly on a child, you'll likely need to kneel on the floor.
- Don't try to pull the object out of the child's mouth if the child is conscious. Try to get it out with the Heimlich maneuver instead.
- You can also place a child across your lap face down, if that is more feasible.
2. Give five back blows
Use the heel of your hand. Whack the child on the back directly between the shoulder blades five times.
- These blows should be fairly hard. They shouldn't be hard enough to knock the child over with your support, but they do need to be relatively sharp.
- The American Heart Association doesn't teach back blows when performing the Heimlich; the Heimlich alone (abdominal thrusts) can be effective without them.
- Look to see if the object has dislodged. You may see the object fly out, or you may notice the child has started breathing again.
3. Place your fists
Put your arms around the child. Use one hand to make a fist and place it directly above the child's navel. Try to get below the breastbone. Cover your fist with the other hand.
4. Pull upward
Pull your fists upward into the child's abdomen. Make this thrust quickly. Repeat four times or until you notice the object choking the child dislodges.
5. Call emergency services (see "EMERGENCY NUMBERS" above)
If no one is around and you've tried the Heimlich once, be sure to call emergency services (see "EMERGENCY NUMBERS" above). You want help to be on the way. If you asked someone else to call emergency services, make sure the person has done it.
6. Check to see if it worked
If it didn't work, continue moving back and forth between back blows and abdominal thrusts. Keep going until you see the object come out, the child begins to breathe normally again, or the child becomes unconscious
Part 3: Helping an Unconscious Choking Child
1. Lay the child on the floor
Once the child loses consciousness, place him on the floor on his back. He should be on a flat, hard surface. Make sure to do so gently.
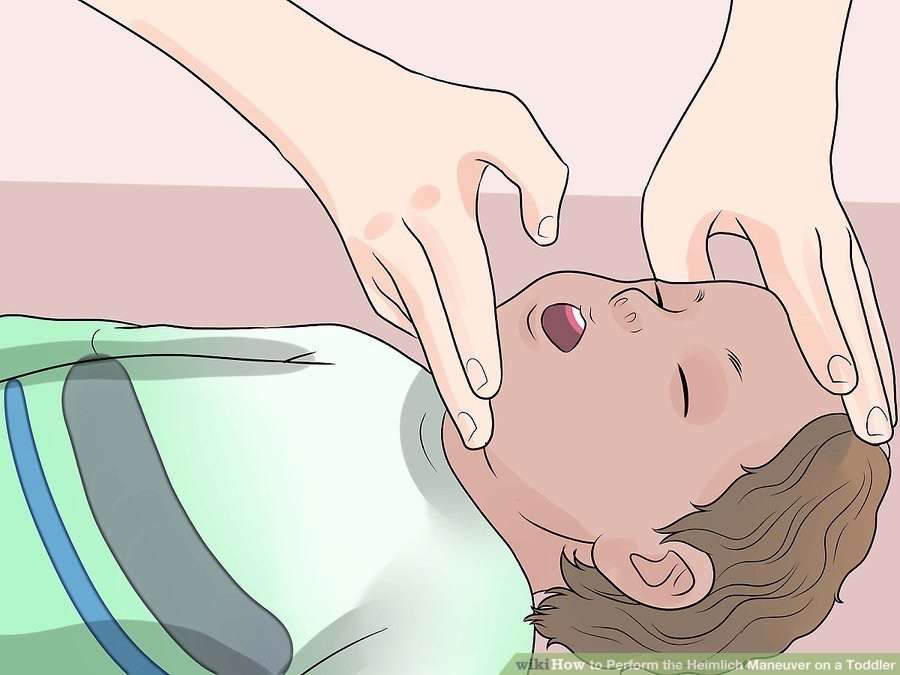
2. Check for an object
Do a sweep of the child's mouth. Gently tilt her head to the side and open her mouth, and use a finger to sweep out an object if you see one. Only try to remove the object if it's loose; if it's stuck in the child's throat, don't try to move it, as you can push it further down.
3. Try two rescue breaths
Tilt the child's head back to open up the airway by lifting the chin. Hold his nose so air can't escape. Cover his mouth with your mouth and blow air in twice, blowing for about a second each time. Watch his chest to see if it rises. If it doesn't, move on to chest compressions.
- If you're having trouble pinching his nose and covering his mouth with yours, you can try to cover his nose and mouth with your mouth.
4. Use chest compressions
Find the correct place by feeling where the bottom of the ribs meet. You should be about an inch above that on the child's chest. Put one hand on top of the other, flat on the chest. The heel of your hand should be in the center of the child's chest. Push the chest about 1/3 of the way down, depth-wise (about 2 inches). Try to go quickly; you should be aiming for 100 compressions a minute. Count to 30 compressions.
5. Check for an object again
Your chest compressions could have dislodged the object that was choking the child. Open her mouth and look. Use your finger to sweep out any object. Check to see if the child is breathing by watching her chest.
6. Continue with CPR
Continue switching between two rescue breaths and thirty chest compressions, checking for an object in the mouth in between. Always remember to tilt the child's chin up for the rescue breaths. Keep going until the child's condition changes or help arrives to take over.
7. Seek immediate medical attention
Even once the child has recovered, take him to the doctor anyway. You want to make sure he/she's suffered no permanent damage.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).