Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Cervical Spondylosis
Also known as "Slipped Disc - Neck" or "Hernaited Disc - Neck"
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Colin Tidy (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Cervical spondylosis / slipped sick is a 'wear and tear' process of the vertebrae and discs in the neck. It is a normal part of ageing and does not cause symptoms in many people. However, it is sometimes a cause of neck pain. Symptoms tend to come and go. Treatments include keeping the neck moving, neck exercises and painkillers. In severe cases, the degeneration may cause irritation or pressure on the spinal nerve roots or spinal cord. This can cause arm or leg symptoms (detailed below). In these severe cases, surgery may be an option.
Understanding the neck
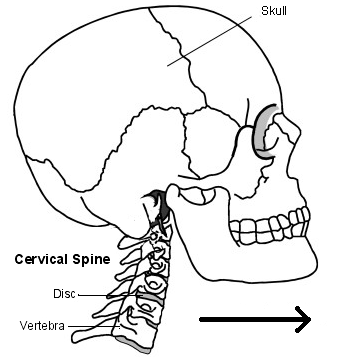
The back of the neck includes the cervical spine and the muscles and ligaments that surround and support it. The cervical spine is made up of seven bones called vertebrae. The first two are slightly different to the rest, as they attach the spine to the skull and allow the head to turn from side to side. The lower five cervical vertebrae are roughly cylindrical in shape - a bit like small tin cans - with bony projections.
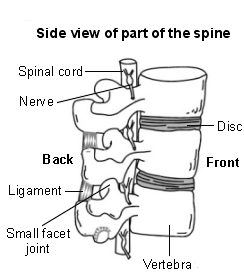
The sides of the vertebrae are linked by small facet joints. Between each of the vertebrae is a 'disc'. The discs are made of a tough fibrous outer layer and a softer gel-like inner part. The discs act like 'shock absorbers' and allow the spine to be flexible.
Strong ligaments attach to adjacent vertebrae to give extra support and strength. Various muscles attached to the spine enable the spine to bend and move in various ways.
The spinal cord, which contains nervous tissue carrying messages to and from the brain, is protected by the spine. Nerves from the spinal cord come out from between the vertebrae in the neck to take and receive messages to the neck and arms. A major blood vessel called the vertebral artery also runs alongside the vertebrae to carry blood to the rear (posterior) part of the brain.
What is cervical spondylosis?
Cervical spondylosis is an age-related degeneration ('wear and tear') of the bones (vertebrae) and discs in the neck. To an extent, we all develop some degeneration in the vertebrae and discs as we become older. It tends to start sometime after the age of about 30.
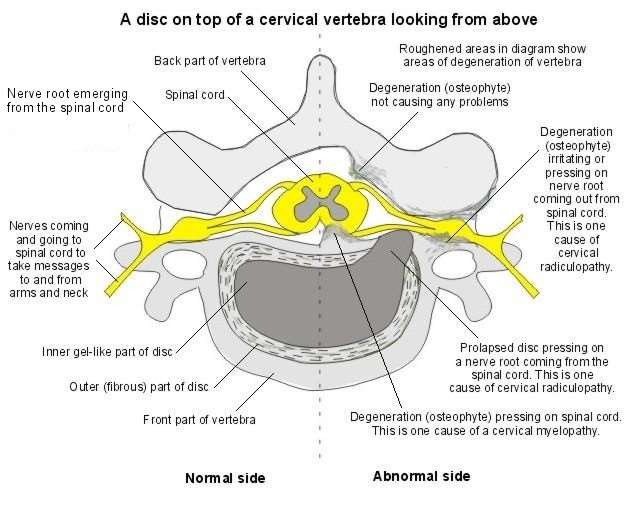
One feature of the degeneration is that the edges of the vertebrae often develop small, rough areas of bone called osteophytes. Also, over many years, the discs become thinner. This degeneration is a normal ageing process which can be likened to having 'wrinkles in the spine'. In many people, the degeneration does not cause any symptoms. For example, routine X-rays of the neck will show these features (osteophytes and disc thinning) in many people who do not have any symptoms.
However, in some people, the nearby muscles, ligaments, or nerves may become irritated or 'pressed on' by the degenerative changes. So, cervical spondylosis often causes no problems but can be a cause of neck pain, particularly in older people.
Symptoms
What are the symptoms of cervical spondylosis?
If symptoms develop, they can range from mild to severe.
Symptoms may include:
Pain and stiffness in the neck:
- This may spread to the shoulders and base of the skull. Movement of the neck may make the pain worse.
- The pain sometimes spreads down an arm to a hand or fingers. This is caused by irritation of a nerve which goes to the arm from the spinal cord in the neck.
- The pain tends to come and go with flare-ups from time to time. You may have a flare-up of pain after unaccustomed use of your neck, or if you sprain a neck muscle or ligament.
- However, a flare-up often develops for no apparent reason. Some people develop chronic (persistent) pain.
- Some neck stiffness, particularly after a night's rest.
- Headaches may occur. The headaches often start at the back of the head just above the neck and travel over the top to the forehead.
- You may develop 'pins and needles' in part of an arm or hand. This symptom is caused by irritation of a spinal nerve as it leaves the bony (vertebral) area. However, do tell a doctor if loss of feeling (numbness) or weakness develops in a part of a hand or arm. These symptoms suggest more pressure on a nerve. This is called a 'cervical radiculopathy'.
- More rarely, clumsiness of a hand, problems with walking, or problems with bladder function occur when pressure from a worn bone (vertebra) or disc damages the spinal cord. This is called 'cervical myelopathy'. Again, it is important to report these symptoms to a doctor.
Note: cervical radiculopathy and cervical myelopathy are discussed further (see below). The following section concerns cervical spondylosis without radiculopathy or myelopathy.
Treatment
What are the treatments for cervical spondylosis without radiculopathy or myelopathy?
Exercise your neck and keep active
Aim to keep your neck moving as normally as possible. During flare-ups the pain may be quite bad, and you may need to rest for a day or so. However, gently exercise the neck as soon as you are able. You should not let it 'stiffen up'. Gradually try to increase the range of the neck movements. Every few hours gently move the neck in each direction. Do this several times a day.
As far as possible, continue with normal activities. You will not cause damage to your neck by moving it.
Medicines
Painkillers are often helpful.
- Paracetamol at full strength is often sufficient.
- Anti-inflammatory painkillers: Some people find that these work better than paracetamol. They can be used alone or in combination with paracetamol. They include ibuprofen which you can buy at pharmacies or obtain on prescription. Other types such as diclofenac or naproxen need a prescription. Some people with stomach ulcers, asthma, high blood pressure, kidney failure, or heart failure may not be able to take anti-inflammatory painkillers.
- A stronger painkiller such as codeine is an option if anti-inflammatories do not suit or do not work well. Codeine is often taken in addition to paracetamol. Constipation is a common side-effect from codeine. To prevent constipation, have lots to drink and eat foods with plenty of fibre.
- A low-dose tricyclic antidepressant, such as amitriptyline, is sometimes used for persistent (chronic) neck pain. The dose of amitriptyline used for pain is 10-30 mg at night. At higher doses, tricyclic antidepressants are used to treat depression. However, at lower doses they have been found to help relieve certain types of pain, including neck pain.
Physiotherapy
If symptoms do not improve over a week or so, you may then be referred to a physiotherapist to help with pain relief and for advice on specific neck exercises.
Various treatments may be advised by a physiotherapist. These include traction, heat, cold, manipulation, etc. The value of each of these treatments is uncertain, as the results of research studies looking at which treatments work best can be conflicting.
However, what is often most helpful is the advice a physiotherapist can give on neck exercises to do at home. A common situation is for a doctor to advise on painkillers and gentle neck exercises.
Other treatments
Some other treatments which may be advised include:
- A good posture may help. Check that your sitting position at work or at the computer is not poor (that is, not with your head flexed forward with a stooped back). Sit upright. Yoga, Pilates and the Alexander Technique all improve neck posture; however, their value in treating neck pain is uncertain.
- A firm supporting pillow seems to help some people when sleeping. Try not to use more than one pillow.
Treatment may vary, and you should go back to see a doctor:
- If the pain becomes worse or severe.
- If other symptoms develop such as loss of feeling (numbness), weakness, or persistent pins and needles in a part of an arm or hand, as described previously.
- If you develop any problems with walking or with passing urine. Again, these symptoms suggest that cervical myelopathy may be developing as a complication of the cervical spondylosis.
- If you develop dizziness or blackouts when turning the head or bending the neck. This can suggest that the vertebral artery which supplies the brain is being nipped by the degenerative changes in the spine.
Other pain-relieving techniques may be tried if the pain becomes chronic. For example, you may be referred to a pain clinic and a pain management programme may be offered to help you control and live with your pain.
Chronic neck pain is also sometimes associated with anxiety and depression which may also need to be treated.
Cervical radiculopathy and cervical myelopathy
Cervical spondylosis is an age-related degeneration ('wear and tear') of the bones (vertebrae) and discs in the neck. It can progress to cause cervical radiculopathy or cervical myelopathy (described below). Most cases do not. However, it may be useful to be aware of the symptoms that suggest they may be happening, particularly as some of them may develop slowly. See a doctor if you suspect that you are developing cervical radiculopathy or cervical myelopathy.
Cervical radiculopathy
This occurs when the root of a nerve is pressed on or damaged as it comes out from the spinal cord in the neck (cervical) region. Although there are other causes of radiculopathy, cervical spondylosis is a common cause.
Degenerative changes to the joints around the vertebrae and osteophyte formation produce areas of narrowing which may nip the nerve. Another cause is a prolapsed disc. This is sometimes called a 'slipped disc' although the disc does not actually slip. What happens is that part of the inner softer area of the disc bulges out (prolapses) through a weakness in the outer harder part of the disc. This presses on the nerve as it passes out between the vertebra.
As well as neck pain, symptoms of radiculopathy include loss of feeling (numbness), pins and needles, pain and weakness in parts of an arm or hand supplied by the nerve. These other symptoms may actually be the main symptoms rather than neck pain. There may be shooting pains down into the arm. The symptoms are usually worse in one arm but may affect both. The pain may be severe enough to interfere with sleep. The lower cervical vertebrae are the usual ones affected, causing these symptoms in the arms. However, if the upper vertebrae are involved, the pain and numbness occur at the back and the side of the head.
Your doctor may suspect a radiculopathy if you have the typical symptoms. A doctor's examination may show changes to the sensation, power and tendon reflexes to areas of the arm supplied by the affected nerve. You may then be referred to a specialist for further tests. These may include an MRI scan which will show whether the nerve roots are being pressed on.
Treatment will depend on how severe the pressure and damage are. In many cases the symptoms settle over time. A course of physiotherapy or a neck collar used for a prescribed period may help. However, in some situations, surgery may be recommended which aims to relieve the pressure on the nerve. Depending on the cause, this may involve surgery to the disc or to the vertebra itself.
Cervical myelopathy
This occurs when there is pressure on or damage to the spinal cord itself. Again, cervical spondylosis is a common cause of this condition, as the degenerative changes to the vertebra can narrow the canal through which the spinal cord passes. A prolapse of a cervical disc can also cause myelopathy if the prolapse is into the central canal of the vertebra. This may happen suddenly or develop over a period of time. There are various other rare causes of cervical myelopathy. For example, a tumour or infection that affects this part of the spinal cord.
As the spinal cord is made up of groups of nerve fibres carrying messages to the brain from the rest of the body, pressure on these nerves in the neck region can produce symptoms from several parts of the body.
The symptoms of a cervical myelopathy may include:
- Difficulties with walking: For example, the legs may feel stiff and clumsy.
- Changes to the sensation of the hands: For example, it may be difficult to feel and recognise objects in the usual way and you may have a tendency to drop things.
- Problems with your bladder: For example, you may experience problems with emptying your bladder, or incontinence.
A doctor's examination may show changes to the sensation, power and tendon reflexes to the legs and arms. You are likely to be referred to a specialist for further tests, usually an MRI scan. This will show how the spinal cord is affected and whether any surgical treatment to relieve the pressure is likely to help.
About the author
Dr Colin Tidy
MBBS, MRCGP, MRCP, DCH
Dr Colin Tidy qualified as a doctor in 1983 and he has been writing for Patient since 2004. Dr Tidy has 25 years’ experience as a General Practitioner. He now works as a GP in Oxfordshire, with a special interest in teaching doctors and nurses, as well as medical students. In addition to writing many leaflets and articles for Patient, Dr Tidy has also contributed to medical journals and written a number of educational articles for General Practitioner magazines.
Recommended websites
For further reading go to:
- Neck Pain – common causes
- Whiplash neck injury – car crash
- Torticollis – sudden onset “frozen” neck pain
- Investigating the spine - the role of a MRI Scan
- Spinal Stenosis – narrowing of the spinal canal
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).