Procedures Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription platform or service. Always refer any concerns or questions about diagnosis, treatment or prescription to your doctor.
Male Sterilisation
Also known as a Vasectomy
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Colin Tidy, reviewed by Dr Hannah Gronow (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is a vasectomy?
Vasectomy is very reliable - but not quite 100%. Even after a successful operation, about 1 in 2,000 men who have had a vasectomy will become fertile again.
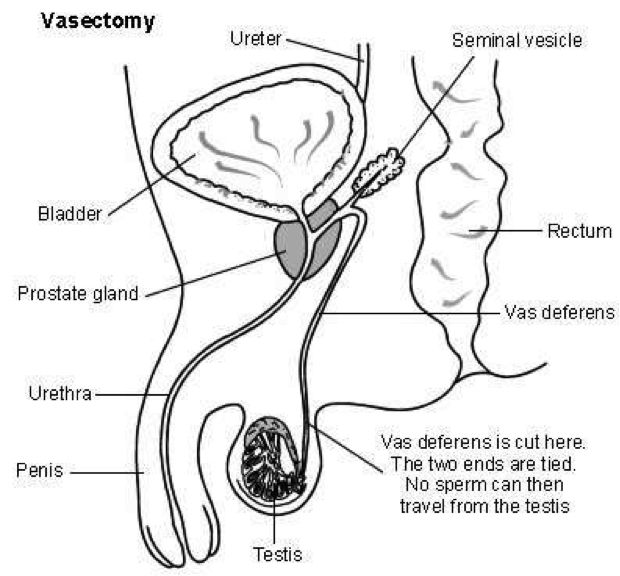
Vasectomy is a small operation to cut the vas deferens. This is the tube that takes sperm from the testicles (testes) to the penis. Sperm are made in the testes. Once the vas deferens is cut, sperm can no longer get into the semen that comes out (is ejaculated) during sex.
How reliable is vasectomy?
Vasectomy is very reliable - but not quite 100%. Even after a successful operation about 1 in 2,000 men who have had a vasectomy will become fertile again at some point in the future. This is because, rarely, the two ends of the cut vas deferens re-unite over time.
In a few cases, operations are not successful and tests show sperm are still present in semen after the operation. This occurs in less than 1 in 100 operations.
How is a vasectomy done?
Cross-section of male reproductive organs, showing vasectomy procedure:
Vasectomy is usually done under a local anaesthetic. This means you are awake but have an injection into the skin so that you do not feel pain. Local anaesthetic is injected into a small area of skin on either side of the scrotum above the testicles (testes). A small cut is then made to these numbed areas of skin. Occasionally vasectomy is done under a general anaesthetic.
A tiny cut or puncture hole is made in the skin on each side of the scrotum. The vas deferens can be seen quite easily under the cut skin. It can be cut with a surgical knife (scalpel) or using diathermy. Diathermy is electrical current that cuts and seals the ends of the tubes. It stops bleeding at the same time. Sometimes a small piece of the vas deferens is removed.
The hole is so small you may not need any stitches. If you do, dissolvable stitches are used, or a special surgical tape. The operation takes about 15 minutes.
There is usually some discomfort and bruising for a few days afterwards. This normally goes away quickly. The discomfort can be helped by wearing tight-fitting underpants day and night for a week or so after the operation. It is also best not to do heavy lifting or strenuous exercise for four weeks or so after the operation.
Are there any risks to the operation?
Most men have no problems after a vasectomy. Problems are uncommon but include the following:
- As with any operation or cut to the skin, there is a small risk of a wound infection.
- The bruising around the operation site is sometimes quite marked. However, it will go in a week or so.
- Rarely, sperm may leak into the scrotum and form a swelling which may need treatment.
- A small number of men have a dull ache in the scrotum for a few weeks or months after the operation. This usually settles within three months.
- A small number of men develop a pain which does not settle over time. This can be mild or severe. It may be in the scrotum, the penis, the testicles (testes) or the lower tummy.
- If you have a general anaesthetic, as with any operation, there is a small risk associated with the anaesthetic.
How do I know it has been successful?
Some sperm survive in the upstream part of the vas deferens for several weeks after vasectomy. These can get into the semen for a while after the operation. About twelve weeks after the operation you will need to produce a semen test. This is looked at under the microscope to check for sperm.
If there are no sperm in this sample, you will be given the all clear. If not, you will need another test a month later. You will be told when the test shows the operation has been successful. Until this time you should continue using another method of contraception.
What are the advantages and disadvantages of vasectomy?
Advantages
It is permanent and you don't have to think of contraception again. It is easier to do and more effective than female sterilisation.
Disadvantages
It may take a few months before the semen is free from sperm. As it is permanent, some people regret having a vasectomy, especially if their circumstances change. Vasectomy does not protect you from sexually transmitted infections.
Will it affect my sex drive?
No. The sex hormones made by the testicles (testes) - for example, testosterone - continue to be passed into the bloodstream as before. Also, vasectomy does not reduce the amount of semen when you come (ejaculate) during sex. Sperm only contribute a tiny amount to semen. Semen is made in the seminal vesicles and prostate higher upstream.
Sex may even be more enjoyable, as the worry or inconvenience of other forms of contraception is removed.
What happens to the sperm?
Sperm are still made as before in the testicles (testes). The sperm cannot get past the blocked vas deferens and are absorbed by the body.
Some other points about vasectomy
Do not consider having the operation unless you and your partner are sure you do not want children, or further children. Consider all sorts of situations, including a tragedy in the family or a break-up of your relationship. Only have a vasectomy if you are sure you would not want more children even in those situations.
It is wise not to make the decision at times of crisis or change, such as after a new baby or termination of pregnancy. It is best not to make the decision if there are any major problems in your relationship with your partner.
Remember there are reversible forms of long-term contraception which are very effective. Consider these as a couple before making your decision. These are all for women.
Ideally, both partners are happy with the decision before a vasectomy. However, it is not legally necessary to obtain your partner's permission.
Some common questions about vasectomy
Does the operation hurt?
No more than any other minor operation that uses local anaesthetic. The injection of local anaesthetic may sting a bit for a few seconds. It is put in just a small area of skin. After this, the operation is usually painless. After the operation, when the local anaesthetic wears off, the top part of the scrotum is normally mildly sore for a few days.
What if I change my mind?
Vasectomy is considered permanent. There is an operation to re-unite the two cut ends of the vas deferens. It is a difficult operation and not always successful.
How soon after the operation can I have sex?
It is recommended to abstain from sex for between 2 to 7 days after the vasectomy. However, remember you will have to use other methods of contraception until your semen specimen has been confirmed as clear of sperm. Some sperm will survive upstream from the cut vas deferens for a few weeks.
I have heard that there is an increase in the risk of prostate cancer after vasectomy. Is this true?
A few studies have shown that there does seem to be an association between vasectomy and a small increased risk of prostate cancer. Guidelines in the UK from the Faculty of Sexual and Reproductive Healthcare (FSRH) state that there is no evidence that vasectomy causes prostate cancer. They consider that it is likely there is another factor which links vasectomy and prostate cancer.
About the author
Dr Colin Tidy
MBBS, MRCGP, MRCP, DCH
Dr Colin Tidy qualified as a doctor in 1983 and he has been writing for Patient since 2004. Dr Tidy has 25 years’ experience as a General Practitioner. He now works as a GP in Oxfordshire, with a special interest in teaching doctors and nurses, as well as medical students. In addition to writing many leaflets and articles for Patient, Dr Tidy has also contributed to medical journals and written a number of educational articles for General Practitioner magazines.
Dr Hannah Gronow
MB ChB
Hannah qualified in 1997. She joined EMIS (patient.info) as a peer reviewer in August 2006. Currently a part time salaried GP in Paignton and moving to a practice in Brixham in 2018. Hannah is about to start a diploma in psychotherapy. Her interests include oncology and pharmacology.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).