Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Boutonnière Deformity
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website OrthoInfo. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is Boutonnière Deformity?
Boutonnière deformity is the result of an injury to the tendons that straightens the middle joint of your finger. The result is that the middle joint of the injured finger will not straighten, while the fingertip bends back. Unless this injury is treated promptly, the deformity may progress, resulting in permanent deformity and impaired functioning.
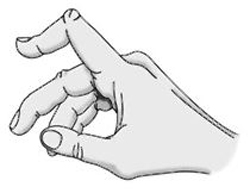
The characteristic shape of Boutonnière deformity. The middle joint of the affected finger will not straighten, while the tip of the finger bends back.
Anatomy
There are several tendons in your fingers that work together to bend and straighten the finger. These tendons run along the side and top of the finger. The tendon on the top of the finger attaches to the middle bone of the finger (the central slip of tendon). When this tendon is injured, the finger is not able to be fully straightened.
Cause
Boutonnière deformity is generally caused by a forceful blow to the top (dorsal) side of a bent (flexed) middle joint of a finger.
It also can be caused by a cut on the top of the finger, which can sever the central slip (tendon) from its attachment to the bone. The tear looks like a buttonhole ("boutonnière" in French). In some cases, the bone actually can pop through the opening.
Boutonnière deformities may also be caused by arthritis.
Symptoms
Signs of boutonnière deformity can develop immediately following an injury to the finger or may develop a week to 3 weeks later.
- The finger at the middle joint cannot be straightened and the fingertip cannot be bent.
- Swelling and pain occur and continue on the top of the middle joint of the finger.
Doctor Examination
Because a boutonnière deformity is only one of several injuries that result from a "jammed finger," you should consult a doctor for an appropriate diagnosis and treatment.
Your doctor will examine the fingers and hand. He or she will ask you to straighten the affected finger and bend the fingertip. X-rays may be recommended to detect any broken bones attached to the central slip of tendon.
Treatment
Boutonnière deformity must be treated early to help you retain the full range of motion in the finger.
Nonsurgical Options
Nonsurgical treatment is usually preferred, and may include:
Splints
A splint will be applied to the finger at the middle joint to straighten it. This keeps the ends of the tendon from separating as it heals. It also allows the end joint of the finger to bend. It is important to wear the splint continuously for the recommended length of time -- usually 6 weeks for a young patient and 3 weeks for an elderly patient. Following this period of immobilization, you may still have to wear the splint at night.
A commercial splint used in treating boutonnière deformity. Splinting helps keep the ends of the tendon from separting during healing.

Exercises
Your physician may recommend stretching exercises to improve the strength and flexibility in the fingers.
Protection
If you participate in sports, you may have to wear protective splinting or taping for several weeks after the splint is removed.
People with boutonnière deformity caused by arthritis may be treated with oral medications or corticosteroid injections, as well as splinting.
Surgical Options
While nonsurgical treatment of boutonnière deformity is preferred, surgery is an option in certain cases, such as when:
- The deformity results from rheumatoid arthritis.
- The tendon is severed.
- A large bone fragment is displaced from its normal position.
- The condition does not improve with splinting.
Surgery can reduce pain and improve functioning, but it may not be able to fully correct the condition and make the finger look normal. If the boutonniere deformity remains untreated for more than 3 weeks, it becomes much more difficult to treat.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).