Conditions Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription service, forum or platform. Always consult your own healthcare practitioner for a more personalised and detailed opinion
Chronic Shoulder Injury
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website OrthoInfo. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is chronic shoulder injury?
The shoulder is the most moveable joint in your body. It helps you to lift your arm, to rotate it, and to reach up over your head. It is able to turn in many directions. This greater range of motion, however, can cause instability.
Shoulder instability occurs when the head of the upper arm bone is forced out of the shoulder socket. This can happen as a result of a sudden injury or from overuse.
Once a shoulder has dislocated, it is vulnerable to repeat episodes. When the shoulder is loose and slips out of place repeatedly, it is called chronic shoulder instability.
Anatomy
Your shoulder is made up of three bones: your upper arm bone (humerus), your shoulder blade (scapula), and your collarbone (clavicle).
Normal shoulder anatomy:
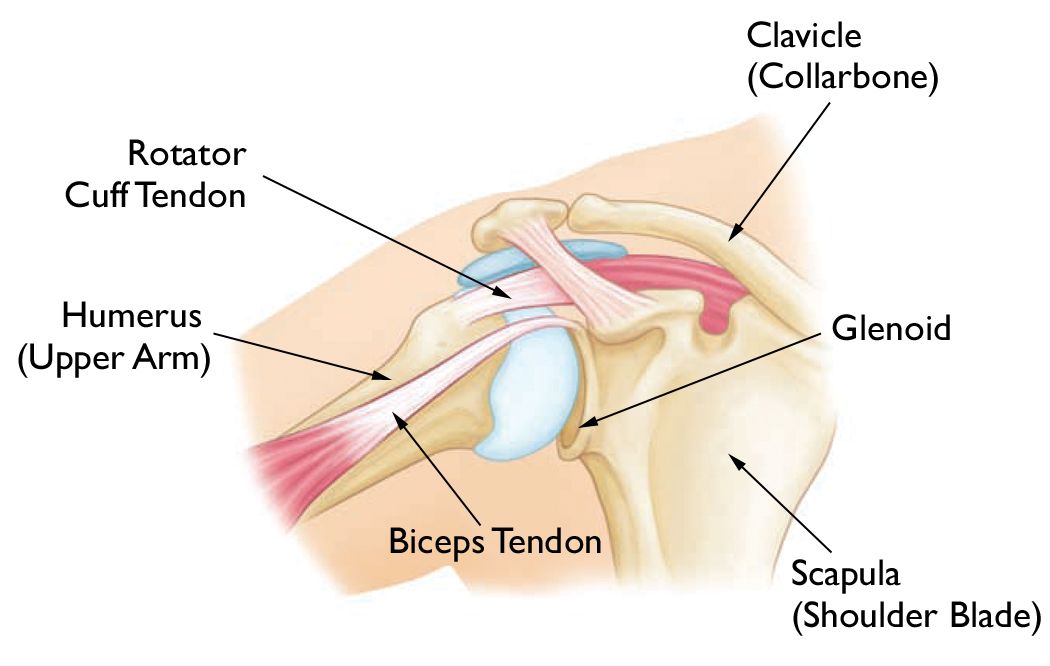
The head, or ball, of your upper arm bone fits into a shallow socket in your shoulder blade. This socket is called the glenoid. Strong connective tissue, called the shoulder capsule, is the ligament system of the shoulder and keeps the head of the upper arm bone centered in the glenoid socket. This tissue covers the shoulder joint and attaches the upper end of the arm bone to the shoulder blade.
Your shoulder also relies on strong tendons and muscles to keep your shoulder stable.
Description
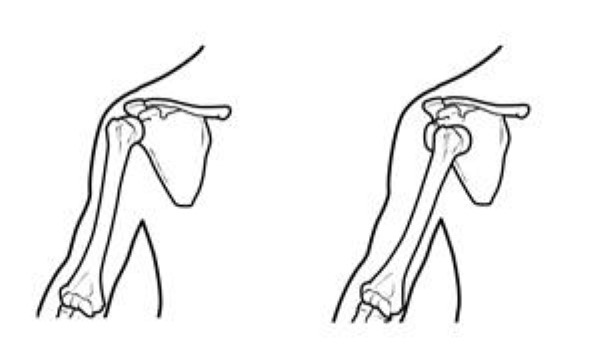
Shoulder dislocations can be partial, with the ball of the upper arm coming just partially out of the socket. This is called a subluxation. A complete dislocation means the ball comes all the way out of the socket.
Once the ligaments, tendons, and muscles around the shoulder become loose or torn, dislocations can occur repeatedly. Chronic shoulder instability is the persistent inability of these tissues to keep the arm centered in the shoulder socket.
(Left) Normal shoulder stability. (Right) Head of the humerus dislocated to the front of the shoulder.
Cause
There are three common ways that a shoulder can become unstable:
Shoulder Dislocation
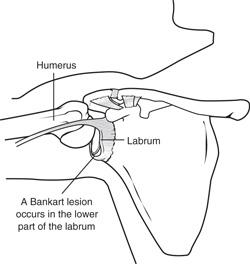
Severe injury, or trauma, is often the cause of an initial shoulder dislocation. When the head of the humerus dislocates, the socket bone (glenoid) and the ligaments in the front of the shoulder are often injured. The labrum — the cartilage rim around the edge of the glenoid — may also tear. This is commonly called a Bankart lesion. A severe first dislocation can lead to continued dislocations, giving out, or a feeling of instability.
A Bankart lesion is a tear in the labrum—the cartilage rim around the edge of the shoulder socket.
Repetitive Strain
Some people with shoulder instability have never had a dislocation. Most of these patients have looser ligaments in their shoulders. This increased looseness is sometimes just their normal anatomy. Sometimes, it is the result of repetitive overhead motion.
Swimming, tennis, and volleyball are among the sports requiring repetitive overhead motion that can stretch out the shoulder ligaments. Many jobs also require repetitive overhead work.
Looser ligaments can make it hard to maintain shoulder stability. Repetitive or stressful activities can challenge a weakened shoulder. This can result in a painful, unstable shoulder.
Multidirectional Instability
In a small minority of patients, the shoulder can become unstable without a history of injury or repetitive strain. In such patients, the shoulder may feel loose or dislocate in multiple directions, meaning the ball may dislocate out the front, out the back, or out the bottom of the shoulder. This is called multidirectional instability. These patients have naturally loose ligaments throughout the body and may be "double-jointed."
Symptoms
Common symptoms of chronic shoulder instability include:
- Pain caused by shoulder injury
- Repeated shoulder dislocations
- Repeated instances of the shoulder giving out
A persistent sensation of the shoulder feeling loose, slipping in and out of the joint, or just "hanging there".
Doctor Examination
Physical Examination and Patient History
After discussing your symptoms and medical history, your doctor will examine your shoulder. Specific tests help your doctor assess instability in your shoulder. Your doctor may also test for general looseness in your ligaments. For example, you may be asked to try to touch your thumb to the underside of your forearm.
Imaging Tests
Your doctor may order imaging tests to help confirm your diagnosis and identify any other problems.
X-rays
These pictures will show any injuries to the bones that make up your shoulder joint.
Magnetic resonance imaging (MRI)
This provides detailed images of soft tissues. It may help your doctor identify injuries to the ligaments and tendons surrounding your shoulder joint.
Treatment
Chronic shoulder instability is often first treated with nonsurgical options. If these options do not relieve the pain and instability, surgery may be needed.
Nonsurgical Treatment
Your doctor will develop a treatment plan to relieve your symptoms. It often takes several months of nonsurgical treatment before you can tell how well it is working.
Nonsurgical treatment typically includes:
- Activity modification: You must make some changes in your lifestyle and avoid activities that aggravate your symptoms.
- Non-steroidal anti-inflammatory medication: Drugs like aspirin and ibuprofen reduce pain and swelling.
- Physical therapy: Strengthening shoulder muscles and working on shoulder control can increase stability. Your therapist will design a home exercise program for your shoulder.
Surgical Treatment
Surgery is often necessary to repair torn or stretched ligaments so that they are better able to hold the shoulder joint in place.
Bankart lesions can be surgically repaired. Sutures and anchors are used to reattach the ligament to the bone.
- Arthroscopy: Soft tissues in the shoulder can be repaired using tiny instruments and small incisions. This is a same-day or outpatient procedure. Arthroscopy is a minimally invasive surgery. Your surgeon will look inside the shoulder with a tiny camera and perform the surgery with special pencil-thin instruments.
- Open Surgery: Some patients may need an open surgical procedure. This involves making a larger incision over the shoulder and performing the repair under direct visualization.
- Rehabilitation: After surgery, your shoulder may be immobilized temporarily with a sling.
When the sling is removed, exercises to rehabilitate the ligaments will be started. These will improve the range of motion in your shoulder and prevent scarring as the ligaments heal. Exercises to strengthen your shoulder will gradually be added to your rehabilitation plan.
Be sure to follow your doctor's treatment plan. Although it is a slow process, your commitment to physical therapy is the most important factor in returning to all the activities you enjoy.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).