Back Conditions Explained
Osteoarthritis
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the Cleveland Clinic, Ohio. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
What is osteoarthritis?
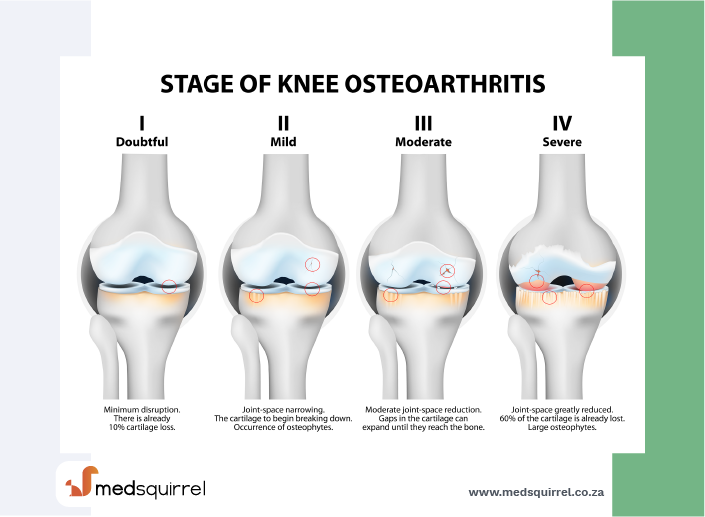
Osteoarthritis, also known as degenerative joint disease or age-related arthritis, is the most common type of arthritis. Osteoarthritis is more likely to develop as people age. The changes in osteoarthritis usually occur slowly over many years, though there are occasional exceptions. Inflammation and injury to the joint cause a breaking down of cartilage tissues, resulting in pain, swelling, and deformity of the joint.
Types of osteoarthritis
There are two main types of osteoarthritis:
- Primary: more generalized osteoarthritis that affects the fingers, thumbs, spine, hips, and knees
- Secondary: osteoarthritis that occurs after injury, such as repetitive or sports-related injury, or inflammation in a joint
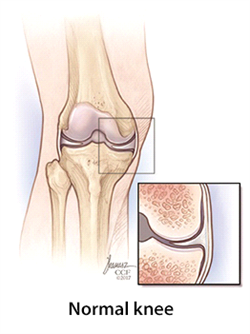
What is cartilage?
Cartilage is a firm, rubbery material covering the ends of bones in normal joints. It is primarily made up of water and proteins whose primary function is to reduce friction in the joints and serve as a "shock absorber." The shock-absorbing quality of normal cartilage comes from its ability to change shape when compressed, because of its high water content. Although cartilage may undergo some repair when damaged, the body does not grow new cartilage after injury.
Cartilage is made up of two main elements: a gel-like substance called matrix, composed mostly of water and two types of proteins (collagen and proteoglycans), and cells known as chondrocytes that are contained within the matrix.
- Collagen is a structural protein found in many tissues such as skin, tendons, and bone, and is a key structural component of cartilage. Collagen provides cartilage with its strength and creates a framework for the other components of cartilage.
- Proteoglycans are complex molecules composed of protein and sugar combinations that are interwoven in the matrix of cartilage. Their function is to trap large amounts of water in cartilage, which allows it to change shape when compressed and thus act as shock absorber.
- Water makes up a large part of healthy cartilage. Water helps to form a "gel-like" matrix with the other components outlined, allowing it to function as the "shock absorber" for the joint. In diseases like osteoarthritis, cartilage loses a lot of its water content. This water loss reduces protection of the joint. Water content may also diminish with age, as older individuals are more prone to having osteoarthritis.
- Chondrocytes are highly complex multifunctional cartilage cells. Functions include production of collagen, proteoglycans, and enzymes, all of which help healthy cartilage grow. As cartilage forms, these cells move through the different layers of cartilage, changing as they do so by mechanisms that are not fully understood.
Who is affected by osteoarthritis?
Although most older individuals (over 60 years old) have evidence of osteoarthritis by X-ray, most people have no symptoms. Women are three times more likely than men to develop primary generalized osteoarthritis. Because age is a risk factor, people are more likely to develop this form of arthritis as they get older.
Causes
What causes osteoarthritis?
Primary generalized osteoarthritis affects women more than men, often occurring shortly after menopause. Most people with primary osteoarthritis have other family members who are affected by the same problem, and usually have swelling and or pain of the finger joints, base of the thumbs, and knees or hips. Secondary osteoarthritis may occur in a joint that was previously injured from trauma, or after the joint has been damaged by some other cause, such as infection or rheumatoid arthritis.
Although the exact mechanisms of cartilage loss and bone changes are unknown, great advancements have been made in recent years. It is likely that complex signalling processes during joint inflammation – and defective repair mechanisms in response to injury – gradually wear down cartilage within the joints. Other changes cause the joint to lose mobility and function, resulting in joint pain with activity.
Risk Factors
Are there other risk factors for osteoarthritis?
In addition to hereditary factors (genes) and other forms of arthritis, several other risk factors increase the risk for developing osteoarthritis, including other hereditary disorders, obesity, and injuries to or around the joint.
Heredity plays a role in osteoarthritis, as individuals born with other diseases are more likely to develop osteoarthritis. Examples include conditions associated with increased joint laxity (being "double-jointed"), some dysplasias (abnormal growths of bone and cartilage), and Paget's disease (a type of inflammation in bone that occurs in older people).
Obesity is a risk factor for osteoarthritis of the lower extremity and spine. Being overweight also may speed the rate of development of osteoarthritis. Maintaining ideal body weight or losing extra weight is important for those at risk.
Injuries (such as those occurring in many athletes) contribute to the development of osteoarthritis. An injury that results in abnormal stress on a joint is another important risk factor for osteoarthritis. Overuse injuries are more controversial, as many people who have similar lifestyles do not develop osteoarthritis. However, repetitive trauma – which may result from overuse – does increase that risk.
Other conditions that may lead to the development of osteoarthritis include peripheral neuropathies (diseases of the nervous system) and neuromuscular disorders that put abnormal stress on the joint.
Diagnosis
How do I know if I have osteoarthritis?
Unlike other types of arthritis, the pain from osteoarthritis usually develops gradually over many months or years. Often it increases with activities that put a lot of stress on the joint, such as running or prolonged walking. Morning stiffness (usually lasting less than 20-30 minutes) is not a prominent symptom as in rheumatoid arthritis or psoriatic arthritis. Pain and joint swelling tend to increase slowly over time. Sometimes, especially in more advanced disease, a sensation of crunching or grinding may be noticed in affected joints.
Osteoarthritis does not usually cause fevers, weight loss, or very hot and red joints. These features suggest some other condition or type of arthritis.
Your doctor or health care provider can usually tell if you have osteoarthritis by listening to your symptoms and examining your joints.
X-rays are helpful to make sure there is no other reason for the pain. Magnetic resonance imaging (MRI) is generally not needed except in unusual circumstances or in cases when a cartilage or surrounding ligament tear is suspected. There are no blood tests that diagnose osteoarthritis. If a joint is particularly swollen, a doctor may need to drain fluid from that joint. Tests can be performed on the fluid to look for clues for other types of arthritis, such as gout.
Treatment
How is osteoarthritis treated?
There is no cure for osteoarthritis. The symptoms usually are managed by a combination of several medical treatments, including medical management for moderate stages and surgery for advanced stages:
- Medications (topical pain medications and oral anti-inflammatories)
- Exercise (land- and water-based)
- Hot and cold packs (local modalities)
- Physical, occupational, and exercise therapy
- Weight loss (if overweight)
- Supportive devices such as crutches, canes, braces, and shoe inserts
- Intra-articular injection therapies (steroid, hyaluronic acid)
- Complementary and alternative medicine strategies
- Surgery may be helpful to relieve pain when other medical treatments are ineffective or have been exhausted.
The goals of treatment are to:
- Decrease joint pain and stiffness and delay further progression
- Improve mobility and function
- Increase patients' quality of life.
The type of treatment regimen prescribed depends on many factors, including the patient's age, overall health, activities, occupation, and severity of the condition.
Medications
Unlike other forms of arthritis where great advances have been made in recent years, progress has been much slower in osteoarthritis. Unfortunately, no medications are available today that have been shown to reverse or slow the progression of osteoarthritis.
Medications are focused on decreasing symptoms of the disease caused by osteoarthritis. Pain-relieving medications include acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and stronger pain medications such as tramadol. Other topical medications in the form of analgesic patches, creams, rubs, or sprays may be applied over the skin of affected areas to relieve pain.
Although many of these medications are available in over-the-counter preparations, individuals with osteoarthritis should talk to a health care provider before taking the medications. Some medications may have dangerous or unwanted side effects and/or may interfere with other medications that are being taken.
Supportive devices
Supportive or assistive devices help decrease stress on affected joints. Bracing and other supports may help to stabilize damaged joints. However, devices should be used sparingly and under the instruction of a health professional such as a therapist, physician, or other health care provider. Relying too much on some supports can lead to muscle wasting, which may make the problem worse. Shoe lifts or inserts and canes or crutches may be helpful to take pressure off certain joints and improve body and gait mechanics.
Exercise
Exercise is important to improve flexibility, joint stability, and muscle strength. Regimens such as swimming, water aerobics, and low-impact strength training are recommended. These have been shown to decrease the amount of pain and disability that osteoarthritis sufferers have. Excessively vigorous exercise programs are best avoided, as they may increase arthritis symptoms and potentially hasten the progression of the disease. Physical therapists or occupational therapists can provide appropriate and tailored exercise regimens for individuals with osteoarthritis.
Hot and cold therapies
Hot and cold treatments may provide temporary relief of pain and stiffness. Such treatments include a hot shower or bath and the careful application of heating or cooling pads or packs.
Weight control
Since obesity is a known risk factor for osteoarthritis, keeping your weight in check may help prevent osteoarthritis. Weight loss in overweight persons who have osteoarthritis has been shown to reduce stress and the amount of pain in weight-bearing joints.
Surgery
When osteoarthritis pain cannot be controlled with medical management and it interferes with normal activities, surgery may be an option. Surgery is usually reserved for those people who have significant osteoarthritis. Several types of techniques can be employed, including minimally invasive joint replacement techniques. Although it has risks, joint surgery today can be very effective at restoring some function and reducing pain for appropriate individuals.
Alternative medicine
Alternative medicine nutraceuticals and supplements are compounds that are available without a prescription and are not licensed by the FDA as drugs. They include nutritional supplements, some vitamins, and other compounds sometimes referred to as "natural," "homeopathic," or "alternative" therapies. Many of these are no more or less "natural" than many prescription medications and may have side effects. It is important to emphasize that because the market for these compounds is less regulated, there is no guarantee that what is on the label is exactly what is in the bottle. Other modalities include acupuncture and stress management.
Glucosamine and chondroitin
Glucosamine and chondroitin are components of normal cartilage. They are most widely available as sulphate compounds. While some clinical trials (particularly in osteoarthritis of the knee) show they may have pain-relieving properties, others have not. Exactly how they work (if they do) remains unclear. There is no strong scientific evidence supporting the claim that they build bone and cartilage.
These nutritional supplements are available in pharmacies and health food stores without a prescription. As this market is less regulated than the food and drug market, many preparations exist, and the actual quantity of ingredients may vary. At least initially, glucosamine and chondroitin appear to be safe and well-tolerated. Whether they have a true impact in the management of osteoarthritis remains to be seen and should be discussed with your physician before starting a trial of nutraceuticals.
Fish oils have some anti-inflammatory activity, but these oils have been studied more extensively for rheumatoid arthritis. Talk to your doctor before using any supplements or treatments.
Recommended websites
For further reading go to:
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
