Back Conditions Explained
Insomnia
Also known as Poor Sleep

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Laurence Knott (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Understanding normal sleep
A normal night's sleep has three main parts:
- Quiet sleep: This is divided into stages 1-4. Each stage becomes progressively more “deep”. Quiet sleep is sometimes called deep sleep.
- Rapid eye movement (REM) sleep: REM sleep occurs when the brain is very active, but the body is limp, apart from the eyes which move rapidly. Most dreaming occurs during REM sleep.
- Short periods of waking for 1-2 minutes.
Each night, about 4-5 periods of quiet sleep alternate with 4-5 periods of REM sleep. In addition, several short periods of waking for 1-2 minutes occur about every two hours or so, but occur more frequently towards the end of the night's sleep. The graph below shows a typical normal pattern of sleep in a young adult.
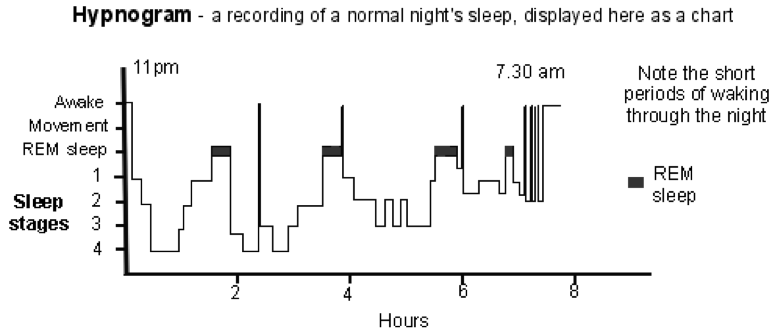
Normally, you do not remember the times that you wake if they last less than two minutes. If you are distracted during the wakeful times (for example, a partner snoring, traffic noise, etc) then the wakeful times tend to last longer, and you are more likely to remember them.
What is insomnia?
Insomnia means poor sleep. About one third of adults do not get as much sleep as they would like.
Poor sleep can mean:
- Not being able to get off to sleep.
- Waking up too early.
- Waking for long periods in the night.
- Not feeling refreshed after a night's sleep.
If you have poor sleep, particularly over a long period of time, it can severely affect your life, as it can cause:
- Tiredness (fatigue) and loss of energy in the daytime.
- Poor concentration.
- Loss of interest in usual activities.
- Irritability.
- Depression and anxiety.
- Inability to do things as well or as much as usual - for example, work, social activities, exercise. Errors might occur at work or whilst driving, which could have serious consequences.
- A worse quality of life.
What is a normal amount of sleep?
Different people need different amounts of sleep. Some people function well and are not tired during the day with just 3-4 hours' sleep a night. Most people need more than this. To need 6-9 hours per night is average. Most people establish a pattern that is normal for them in their early adult life. However, as you become older, it is normal to sleep less. For most people it takes less than thirty minutes to fall asleep.
So, everyone is different. What is important is that the amount of sleep that you get should be sufficient for you, and that you usually feel refreshed and not sleepy during the daytime.
Therefore, the formal medical definition of insomnia is:
'Difficulty in getting to sleep, difficulty staying asleep, early wakening, or non-restorative sleep despite adequate time and opportunity to sleep, resulting in impaired daytime functioning, such as poor concentration, mood disturbance, and daytime tiredness.'
Causes of insomnia
Poor sleep may develop for no apparent reason. However, there are a number of possible causes which include the following:
Concern about wakefulness
You may remember the normal times of being awake in the night. You may feel that to wake in the night is not normal and worry about getting back off to sleep. You may clock-watch and check the time each time you wake up. This may make you irritated or anxious, and you are more likely to remember the times of wakefulness. You may then have an impression of having a bad night's sleep, even when the total amount of time asleep was normal.
Temporary problems
Poor sleep is often temporary. This may be because of stress, a work or family problem, jet lag, a change of routine, a new baby, a strange bed, etc. Poor sleep in these situations usually improves in time.
Stress, anxiety or depression
You may find it difficult to switch off your anxieties about work, home or personal problems. Also, poor sleep is sometimes due to depression. Other symptoms of depression include a low mood, lethargy, poor concentration, tearfulness and persistent negative thoughts. Depression is common. Treatment of depression or anxiety often cures the poor sleep too.
Sleep apnoea
This sometimes occurs in people who snore, most commonly in obese people. In this condition the large airways narrow or collapse as you fall asleep. This not only causes snoring but also reduces the amount of oxygen that gets to the lungs. This causes you to wake up to breathe properly. You may wake up many times each night which may result in daytime tiredness. Note: most people who snore do not have sleep apnoea and they do sleep well.
Other illnesses
Various illnesses keep some people awake. For example, illness causing pain, leg cramps, breathlessness, indigestion, cough, itch, hot flushes, mental health problems, etc.
Stimulants
These can interfere with sleep.
There are three common culprits:
- Alcohol: many people take an alcoholic drink to help sleep. Alcohol actually causes broken sleep and early morning wakefulness.
- Caffeine: which is in tea, coffee, some soft drinks such as cola, and even chocolate. It is also in some painkiller tablets and other medicines (check the ingredients on the medicine packet). Caffeine is a stimulant and may cause poor sleep.
- Nicotine (from smoking): is a stimulant, so it would help not to smoke.
Street drugs
Street drugs (for example, ecstasy, cocaine, cannabis and amfetamines) can affect sleep.
Prescribed medicines
Some medicines sometimes interfere with sleep. For example, 'water tablets' (diuretics), some antidepressants, steroids, beta-blockers, painkillers containing caffeine, and some cold remedies containing pseudoephedrine. Also, if you suddenly stop taking regular sleeping tablets or other sedative medicines, this can cause rebound poor sleep.
Screen time
There is some evidence that the time we spend looking at electronic screens can affect our sleep. It may be that certain types of light from e-readers and electronic tablets can disrupt control of our natural day-and-night cycle. There are studies which suggest we may sleep better after reading a printed book or a particular kind of screen before bedtime. There are also some studies which show that in children and adolescents, more time using electronic devices in the daytime is linked to less good sleep at night. There is not yet enough evidence to make definite recommendations, but it may be worth considering.
Unrealistic expectations
Some people just need less sleep than others. If your sleep pattern has not changed, and you do not feel sleepy during the day, you are probably getting enough sleep. Older people and people who do little exercise tend to need less sleep. Some people think they should be able to nap during the day - and sleep eight hours at night!
A vicious cycle
Whatever the initial cause, worry about poor sleep and worry about feeling tired the next day, are common reasons for the problem to become worse.
Sleep paralysis
Some people may also experience waking from sleep but then being unable to move or speak for a period of time. Some people experience the same problems when they are falling asleep (see below).
Some classifications
There are different definitions and classifications of poor sleep (insomnia) around, which can make things confusing.
Doctors may classify insomnia into one of the following categories:
1. By type
- Primary insomnia is insomnia that occurs when no illness or other secondary cause (comorbidity) is identified. Primary insomnia accounts for about one in five cases of long-term insomnia.
- Secondary (or comorbid) insomnia occurs when insomnia is a symptom of, or is associated with, other conditions. These can be medical or mental health conditions, or drug or substance misuse (as discussed above).
2. By duration
- Short-term if insomnia lasts between one and four weeks.
- Long-term (or persistent) if insomnia lasts for four weeks or longer.
3. By a combination of factors
Some authorities use the term 'chronic insomnia disorder'. To have this diagnosis, you would:
- Have problems sleeping for at least three nights a week for at least three months.
- Be distressed or have problems functioning due to your sleeping problem.
- Not have another condition which could affect sleep, ie mental or physical illnesses or another sleep disorder.
How can I sleep better?
- Avoid caffeine, smoking and alcohol, especially in the hours before bedtime.
- Avoid heavy meals or strenuous exercise shortly before going to bed.
- Go to bed and get up at the same time each day.
- Regular daytime exercise helps you feel more relaxed and tired at bedtime.
This section will discuss five topics which can help to promote better sleep:
- Understanding some facts.
- Sleep hygiene.
- Relaxation techniques.
- Daytime exercise.
- Psychological treatments called cognitive and behavioural therapies.
- In effect, these can be used in a step-wise fashion. You need only go on to the next step if the previous step is not very helpful, but each step requires a greater degree of effort.
Understanding some facts
It is often helpful to understand that short periods of waking each night are normal. Some people are reassured about this and so do not become anxious when they find themselves awake in the night. Also, remember that worry about poor sleep can itself make things worse. Also, it is common to have a few bad nights if you have a period of stress, anxiety or worry. This is often just for a short time and a normal sleep pattern often resumes after a few days.
General tips for sleeping better (often called sleep hygiene)
The following are commonly advised to help promote sleep in people with sleep difficulties, and may be all that is necessary:
Reduce caffeine: do not have any food, medicines, or drinks that contain caffeine or other stimulants for six hours before bedtime (see above). Some people have found that cutting out caffeine completely through the day has helped.
Do not smoke within six hours before bedtime.
Do not drink alcohol within six hours before bedtime.
Do not have a heavy meal just before bedtime (although a light snack may be helpful).
Do not do any strenuous exercise within four hours of bedtime (but exercising earlier in the day is helpful).
Body rhythms - try to get into a routine of wakefulness during the day and sleepiness at night. The body becomes used to rhythms or routines. If you keep to a pattern, you are more likely to sleep well. Therefore:
- No matter how tired you are, do not sleep or nap during the day.
- It is best to go to bed only when sleepy-tired in the late evening.
- Switch the light out as soon as you get into bed.
- Always get up at the same time each day, seven days a week, however short the time asleep. Use an alarm to help with this. Resist the temptation to lie in - even after a poor night's sleep. Do not use weekends to catch up on sleep, as this may upset the natural body rhythm that you have got used to in the week.
The bedroom should be a quiet, relaxing place to sleep:
- It should not be too hot, cold, or noisy.
- Earplugs and eye shades may be useful if you are sleeping with a snoring or wakeful partner.
- Make sure the bedroom is dark with good curtains to stop early morning sunlight.
- Don't use the bedroom for activities such as work, eating or television.
- Consider changing your bed if it is old, or not comfortable.
- Hide your alarm clock under your bed. Many people will clock-watch and this does not help you to get off to sleep.
Mood and atmosphere - try to relax and wind down with a routine before going to bed. For example:
- A stroll followed by a bath, some reading, and a warm drink (without caffeine) may be relaxing in the late evening.
- Do not do anything mentally demanding within 90 minutes of going to bed - such as studying.
- Go to bed when sleepy-tired.
- Some people find playing soft music is helpful at bedtime. Try a player with a time switch that turns the music off after about 30 minutes.
If you cannot get off to sleep after 20-30 minutes - then get up: If you can, go into another room, and do something else such as reading or watching TV rather than brooding in bed. Go back to bed when sleepy. You can repeat this as often as necessary until you are asleep.
Relaxation techniques
These aim to reduce your mental and physical arousal before going to bed. Relaxation techniques may help even if you are not anxious but find it hard to get off to sleep. There are a number of techniques. For example, progressive muscular relaxation has been shown to help promote sleep. This technique consists of tensing and relaxing various muscle groups in sequence.
Your GP or a counsellor may be able to recommend a CD that takes you through deep-breathing exercises, and other methods to help you relax.
Daytime exercise
Regular daytime exercise can help you to feel more relaxed and tired at bedtime. This may help you to sleep better. (However, you should not do exercise near to bedtime if you have insomnia). If possible, do some exercise on most days. Even a walk in the afternoon or early evening is better than nothing. However, ideally, you should aim for at least 30 minutes of moderate exercise on five or more days a week.
Moderate exercise means that you get warm and slightly out of breath. You do not need to go to a gym! Brisk walking, jogging, cycling, climbing stairs, heavy DIY, heavy gardening, dancing and heavy housework are all moderate-intensity physical exercises.
Behavioural and cognitive therapies
If you have severe persistent poor sleep, your doctor may refer you to a psychologist or other health professional for psychological treatments. These are various therapies which help re-train your brain and the way you feel, think or behave. Research studies have found that there is a good chance that behavioural and cognitive therapies will improve sleep in adults with insomnia. Increasingly, research has also shown that some of these therapies can be delivered digitally (i.e. through an app, online, etc).
There are various types of therapy and they include the following:
Stimulus-control therapy. This helps you to re-associate the bed and bedroom with sleep and to re-establish a consistent sleep/wake pattern.
Sleep restriction therapy. Very briefly, the principle of this treatment is that you limit the time that you spend in bed at night. As things improve, the time in bed is then lengthened. An example of the way that this may be done in practice is as follows:
- First, you may be asked to find out how much you are actually sleeping each night. You can do this by keeping a sleep diary.
- You may then be advised to restrict the amount of time that you spend in bed to the time that you actually sleep each night. For example, if you spend eight hours in bed each night but you sleep for only six hours then your allowed time in bed would be six hours. So, in this example, say you normally go to bed at 11 pm, get to sleep at 1 am and get up at 7 am. To restrict your time in bed to six hours, you may be advised to go to bed at 1 am but still get up at 7 am.
- You then make weekly adjustments to the allowed time in bed, depending on the time spent asleep. (You need to keep on with the sleep diary.)
- When 90% of the time spent in bed is spent asleep then the allowed time spent in bed is increased by 15 minutes, by going to bed 15 minutes earlier. In the above example, you would then go to bed at 12.45 am.
- Adjustments are made each week until you are sleeping for a longer length most nights.
Relaxation training: This teaches you ways of reducing tension. For example, this may include the progressive muscle relaxation technique as described earlier, plus various other techniques described earlier.
Paradoxical intention: This involves staying passively awake, avoiding any intention to fall asleep. It is used for people who have trouble getting to sleep (but not maintaining sleep).
Biofeedback: With this technique, you are connected to electrical sensors which give you feedback by sounds and lights to show you what your body is doing. This is to help you control certain body functions (such as muscle tension).
Cognitive therapy: Briefly, cognitive therapy is based on the idea that certain ways of thinking can trigger or fuel certain health problems, such as poor sleep. The therapist helps you to understand your thought patterns. In particular, to identify any harmful or unhelpful ideas or thoughts which you have that can contribute to you not sleeping well. The aim is then to change your ways of thinking and/or behaviour to avoid these ideas. Also, to help your thoughts to be more realistic and helpful. Cognitive therapy is often used in combination with a behavioural intervention (such as stimulus control, sleep restriction, or relaxation training); this is then called cognitive behavioural therapy (CBT).
What about sleeping tablets?
Sleeping tablets are not usually advised
Sleeping tablets should ideally be taken as a last resort. The main types of sleeping tablets are in a class of medicines called benzodiazepines and a class called Z drugs.
In the past, sleeping tablets were commonly prescribed. However, they have been shown to have problems and are now not commonly prescribed, and certain others, the long acting ones especially, have been withdrawn.
Possible problems with sleeping tablets include:
- Drowsiness the next day. You may not be safe to drive or to operate machinery.
- Clumsiness and confusion in the night if you have to get up. For example, if you have had a sleeping tablet, you may fall over if you get up in the night to go to the toilet. (Older people who take sleeping tablets have an increased risk of falling and breaking their hip.)
- Tolerance to sleeping tablets may develop if you take them regularly. This means that, in time, the usual dose has no effect. You then need a higher dose to help with sleep. In time, the higher dose then has no effect, and so on.
- Some people become addicted to (dependent on) sleeping tablets and have withdrawal symptoms if the tablets are stopped suddenly.
Sometimes a sleeping tablet is advised
If a sleeping tablet is prescribed, it is usually just a short course (a week or so) to get over a particularly bad patch. Sometimes a doctor will advise sleeping tablets to be taken on only two or three nights per week, rather than on every night. This prevents tolerance or dependence to the tablet from developing. Learn more about the role of sleeping tablets in insomnia.
Melatonin
Melatonin is, strictly speaking, not a sleeping tablet. Melatonin is a naturally occurring hormone made by the body. The level of melatonin in the body varies throughout the day. It is involved in helping to regulate the daily cycles (circadian rhythms) of various functions in the body. A melatonin supplement is sometimes advised in older people (more than 55 years of age) with persistent insomnia. The recommended duration of treatment is for three to ten weeks only.
Antihistamines
Some of the older, first generation antihistamines can make you sleepy as a side effect and are sold over the counter for this purpose. These should only be used for short periods of time. This is because if you use them for a long-time insomnia can be worse when they are stopped. They can make you excessively sleepy the next day. Also, there is not much evidence about how well they work.
Valerian and other herbal remedies
Herbal remedies are used by some people to help with sleep. For example, valerian. However, research studies have shown that there is very little evidence to show that they work.
A final note
See a doctor if you feel that illness or medication is causing poor sleep. Treating any underlying condition that is causing the problem, if possible, can help to promote sleep. In particular, depression and anxiety are common causes of poor sleep and can often be treated.
About the author
Dr Laurence Knott
BSc (Hons) (Biochemistry), MB BS
Qualified 1973. 37 years experience in general practice. Medical author who has contributed to many lay and professional publications. Particularly interested in converting medical terminology into information comprehensive to non-medical readers. Clinical complaints adviser to the Medical Defence Union. External professional adviser to the Health Service Ombudsman. Extensive medicolegal practice specialising in clinical negligence. Listed on the National Crime Database, advising police forces and the Crown Prosecution Service on medicolegal aspects of criminal cases. Erstwhile GP medical adviser to the Guillain-Barré & Associated Inflammatory Neuropathies charity, now member and ex-patient.
Recommended websites
For further reading go to:
- Relaxation Exercises for better sleep
- Sleeping Tablets – the basics
- Benzodiazepines and Z Drugs – how do they work?
- Sleep Paralysis – more common than previously thought
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
