Back Conditions Explained
Back Pain in Children
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website OrthoInfo. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is back pain in children?
Back pain in children is not like back pain in adults. Compared to an adult, a child with a backache is more likely to have a serious underlying disorder. This is especially true if the child is 4 years old or younger, or if a child of any age has back pain accompanied by:
- Fever or weight loss
- Weakness or numbness
- Trouble walking
- Pain that radiates down one or both legs
- Bowel or bladder problems
- Pain that keeps the child from sleeping
More serious causes of back pain need early identification and treatment or they may become worse. Always see a doctor if your young child's back pain lasts for more than several days or progressively worsens.
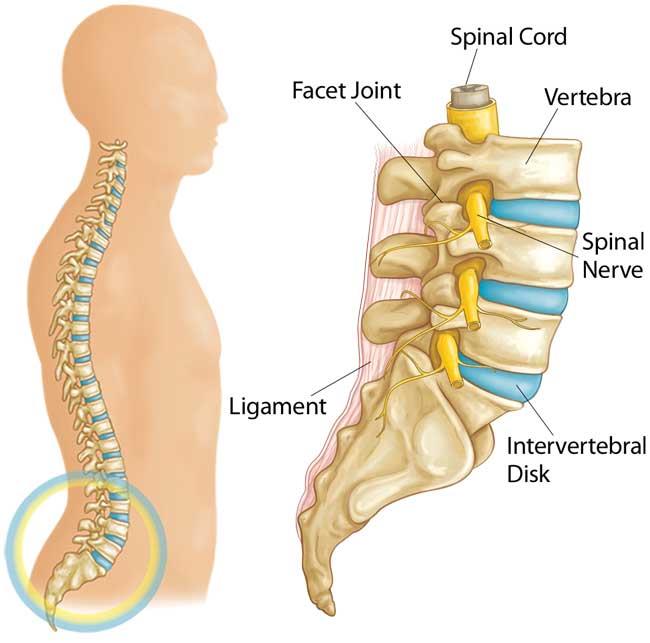
Your spine is made up of small bones, called vertebrae, which are stacked on top of one another and create the natural curves of your back:
Doctor Examination
Your doctor will begin by learning about how the problem developed, and then will conduct a physical examination of your child.
Medical History
Your doctor will ask general questions about your child's overall health and more specific questions about the pain. The questions and physical examination will allow your doctor to determine which of a number of conditions is responsible for your child's back pain.
Your doctor will want to know when the pain began, if it was associated with injury or demanding activity, and whether it has improved or worsened. He or she will ask whether there is anything that makes it worse, and what your child does to make it less painful. It will be important for your doctor to know exactly where the pain is felt, how severe it is, and how much it interferes with the child's schooling and activities. If the pain shoots into a leg it could mean that there is pressure on a nerve.
Physical Examination
During the physical examination, your doctor carefully examines your child's muscles, bones, and nerves.
Your doctor will be checking the following:
The spine
Your doctor feels each vertebra and looks for deformities in the alignment and mobility of the spine. Increased roundness of the back (when viewed from the side) or a curve to the side (when viewed from the back) could be important. Your doctor will check posture and walking gait, the ability to bend over to touch the toes, and bending to the right and left. Difficulty with movement may indicate that there is a problem with the joints of the spine.
Nerves in the back
Problems with the intervertebral disks can cause pressure on the nerves that exit the spine, so your doctor will perform specific tests for that. With your child lying face up, your doctor will raise the legs (straight leg raising test) and may also raise the legs with your child lying face down (reverse straight leg raising test). Testing reflexes and feeling in the legs will be done for the same reason.
Muscles
The muscles in the back and legs are tested. Tightness of the back muscles or the hamstring muscles at the back of the thigh will show that your child is trying to protect himself or herself from movements and positions that might be painful. Tenderness of the muscles will indicate a muscle injury, such as a strain.
Balance, flexibility, coordination, and muscle strength
Other tests may be done to be sure the back pain is not part of a bigger picture.
Imaging Tests
The doctor may use one or several diagnostic imaging tools to see inside the body.
X-rays
X-rays of the spine will show the bones and may show fractures, displacements, or other problems within the bones.
Bone scans
This test involves injecting a substance into a vein and then using a special camera to see where it is picked up. It can pinpoint inflammation, infections, tumors, and fractures. Since the anatomy of the spine is very complicated and since these disease processes are not always visible on x-ray, the bone scan can be very useful.
Computed tomography (CT) scans
This is a special computerized x-ray technique that provides a three-dimensional image and allows your doctor to see things that are not visible on two-dimensional x-rays. It is particularly useful in the spine to understand the complex anatomy.
Magnetic resonance imaging (MRI)
This technique is very valuable because it shows tissues other than bone. It can be used to see the spinal cord, nerve roots, disks, or other soft tissues than can be very important in back pain.
Positron emission tomography (PET)
This test can be a useful adjunct by providing a three-dimensional image of functional processes in the body.
Laboratory Tests
Blood tests, including the complete blood-cell count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), can be affected by the presence of inflammation or infection.
Common Back Pain Conditions in Children
Muscle Strain and Imbalances
Musculoskeletal strain is most often responsible for back pain in children and adolescents. This type of pain frequently responds to rest, anti-inflammatory medications, and an exercise program.
Many teenagers may have more persistent back pain. This is often related to tight hamstring muscles and weak abdominal muscles. These children seem to improve with a physical therapy program that stresses hamstring stretching and abdominal strengthening.
Rounded Back
In adolescents, increased roundness of the back (when viewed from the side) — also called Scheuermann's kyphosis — is a common cause of pain in the middle of the back (the thoracic spine). Vertebrae become wedged, causing a rounded, or hunched, back. The curved part of the back may ache and pain may get worse with activity.
An adolescent male presents with excessive roundback localized to the thoracic spine. The severe kyphosis is most obvious when he bends forward.

Courtesy of Texas Scottish Rite Hospital for Children
Stress Fracture of the Spine
Spondylolysis, or stress fracture, may cause lower back pain in adolescents. Stress fractures may occur during adolescent growth spurts or in sports that repeatedly twist and hyperextend the spine, like gymnastics, diving, and football.
Pain is usually mild and may radiate to the buttocks and legs. The pain feels worse with activity and better with rest. A child with spondylolysis may walk with a stiff legged gait and only be able to take short steps.
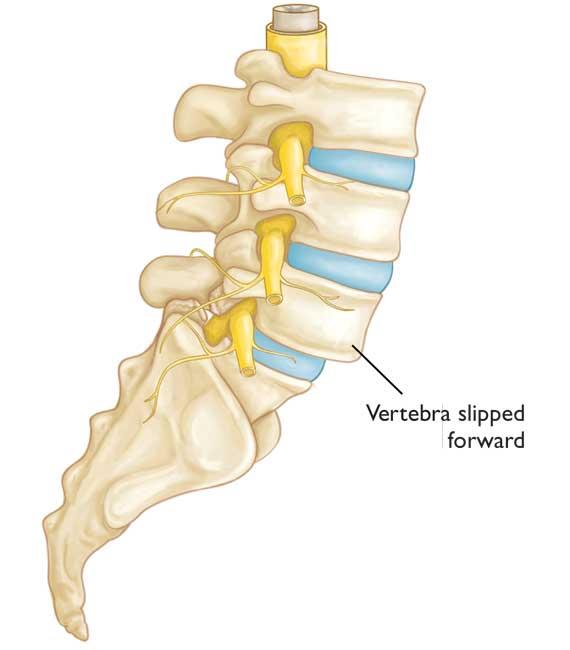
Slipped Vertebra
A slipped vertebra, or spondylolisthesis, occurs when one vertebra shifts forward on the next vertebra directly below. This may sometimes represent progression of a spondylolysis. It usually occurs at the base of the spine (lumbosacral junction). In severe cases, the bone narrows the spinal canal, which presses on the nerves.
In this drawing of spondylolisthesis, a lower back vertebra has shifted forward:
Infection
In young children, infection in a disk space (diskitis) can lead to back pain. Diskitis typically affects children between the ages of 1 and 5 years, although older children and teenagers can also be affected.
A child with diskitis may have the following symptoms:
- Pain in the lower back or abdomen and stiffness of the spine
- Walking with a limp, or simply refusing to walk
- Squatting with a straight spine when reaching for something on the floor, rather than bending from the waist
Tumor
On rare occasion, tumors, such as osteoid osteoma, can be responsible for back pain. When they occur, tumors of the spine are most often found in the middle or lower back. Pain is constant and usually becomes worse over time. This pain is progressive; it is unrelated to activity and/or happens at night.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
