Back Conditions Explained
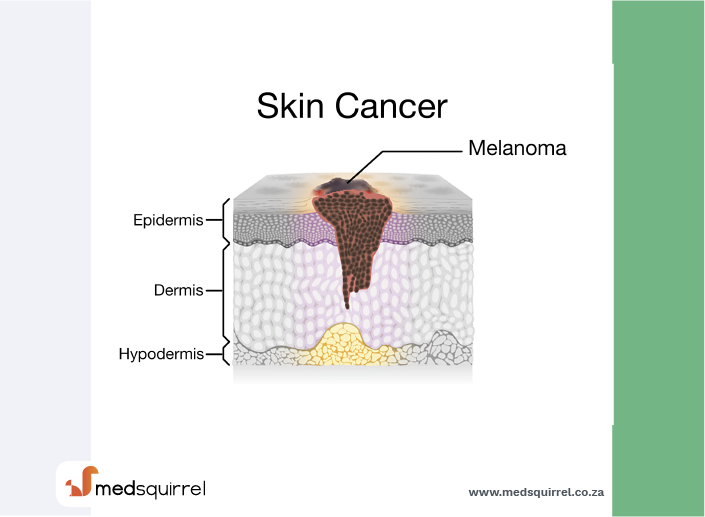
Skin Cancer - Melanoma

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Colin Tidy (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Melanoma is the most serious type of skin cancer. It affects young adults as well as older people. If diagnosed at an early stage, before it has spread, treatment is likely to be curative. The outlook (prognosis) is not so good if it has spread before being treated. See your doctor if you develop an abnormal patch of skin or a change in appearance of a mole.
How common is melanoma?
Melanoma is the least common form of skin cancer, but it is the most serious. It is the one most likely to spread to other parts of the body. There are about 9,000 new cases of melanoma each year in the UK. The number of cases has about doubled over a period of 20 years or so. Melanoma is the second most common cancer in people aged 15-34.
Causes
What causes melanoma?
A cancerous tumour starts from one abnormal cell. The exact reason why a cell becomes cancerous is unclear. It is thought that something damages or alters certain genes in the cell. This makes the cell abnormal and multiply out of control.
Sun or sunbed damage to skin
The main risk factor which damages skin and can lead to a melanoma is damage from the sun. It is the ultraviolet (UV) radiation in the sunshine and in sunbeds which does the damage. About 6 in 10 cases of melanoma are thought to be caused by UV damage. UV light damages the DNA (genetic material) in your skin cells which can then lead to skin cancers developing.
People most at risk of UV skin damage are people with fair skin - in particular, those with skin which always burns and never tans, red or blond hair, green or blue eyes. Melanoma is uncommon in dark-skinned people, as they have more protective melanin in their skin.
Children's skin is most vulnerable to damage. Sun exposure in childhood is the most damaging. People who had a lot of freckling in childhood, or had frequent or severe sunburn in childhood, are most at risk of developing melanoma as adults. (The damage to the skin can occur many years before a cancer actually develops).
Melanoma is most common in fair-skinned people who live in hot countries nearer to the equator. Australia and Israel have the highest rates. The rate in the USA is quite high but decreases the further north you go in the country.
Other risk factors
Other factors which increase the risk of developing melanoma include the following:
A family history: If a close blood relative develops melanoma then your risk is approximately doubled. This increased risk may be due to a shared family lifestyle of frequent sun exposure and/or having fair skin. It may also be due to inherited faulty genes. Around one in ten people with melanoma will have a relative who has also had a melanoma. Further research aims to clarify the role of these and other genes which may be involved. Gene testing for melanoma is not yet possible. As a rule, if you have a family history of melanoma you should take extra care to protect your skin from sun damage. Also, check your skin regularly for early signs of melanoma (see below).
Having many moles: These are the small brown marks which occur on almost everybody. They are caused by a collection of melanocytes in the skin surface. If you have many (especially 100 or more) you have an increased risk that one will develop into a melanoma.
Atypical (non-typical) moles: People with moles which are bigger than usual, with an irregular shape or colour (called atypical), have an increased risk. These moles (sometimes called dysplastic naevi) rarely change into melanoma but it's important to keep an eye on them. If you have a strong family history of melanoma (father, mother, brother or sister with a melanoma) and you have an atypical mole, you have a high risk of developing melanoma. Make sure you check your skin regularly.
Using sunbeds or similar tanning machines which emit UV light: Damage caused by sunbeds seems to be worse in people with red hair and freckles and also in young people under the age of 20 years.
Having a weakened immune system (for example, due to HIV infection, or if you are taking immunosuppressive medicines, perhaps after an organ transplant) then you have an increased chance of getting a melanoma.
Signs & Symptoms
What are the signs of melanoma?
A typical melanoma starts as a small dark patch on the skin. It can develop from a normal part of skin, or from an existing mole.
A melanoma is often different to a mole in one or more of the following ways (summed up as ABCDE) - that is:
- Asymmetry: the shape of a melanoma is often uneven and asymmetrical, unlike a mole which is usually round and even.
- Border: the border or edges of a melanoma are often ragged, notched or blurred. A mole has a smooth well-defined edge.
- Colour: the colour (pigmentation) of a melanoma is often not uniform. So there may be 2-3 shades of brown or black. A mole usually has one uniform colour.
- Diameter: the size of a melanoma is usually larger than 6 mm and it continues to grow. However, they can sometimes be smaller than this.
- Evolving: any change in size, shape, colour, or elevation or any new symptom such as bleeding, itching or crusting may be due to a melanoma.
However, some melanomas are not dark, and some melanomas are not typical in how they look. Melanomas start off small and grow - so smaller size doesn't rule out melanoma. As a melanoma grows in the skin it may itch, bleed, crust or ulcerate.
The take home message is: see a doctor if you develop a lump or patch on the skin, which you are unsure about, or if a mole changes in its shape, border, colour or size.
A melanoma can develop on any area of skin. The most common place for a melanoma to develop in a woman is on the legs; whereas for men it is on the chest or back. Rarely, a melanoma can develop in the iris or back of the eye. (Unlike non-melanoma skin cancers, melanomas can develop on areas of skin not often exposed to the sun. These areas may have had short spells of sun damage such as during a holiday).
If some cells break off and spread (metastasise) to other parts of the body, various other symptoms can develop. A common early symptom of spread is for the nearby lymph glands (nodes) to swell.

Diagnosis
How is a melanoma diagnosed?
If a melanoma is suspected then your doctor is likely to advise an excisional biopsy. In this procedure, the entire abnormal area of skin is removed by a minor operation. (Local anaesthetic is injected into the skin to make this painless.) This tissue is looked at under the microscope. This is to:
- Confirm the diagnosis - abnormal melanoma cells can be seen.
- To assess the melanoma's thickness (how deep it has spread into the skin). The thickness of the melanoma helps to guide treatment and the need for further assessment.
Treatment
Initial treatment and assessment of melanoma
The excisional biopsy may be curative
When doing an excisional biopsy (described above), the doctor will remove a margin of normal skin around the melanoma. When the biopsy is looked at under the microscope, if the doctor is sure that all the melanoma cells have been removed and the melanoma cells are confined to the top layer of skin, no further treatment may be needed. Otherwise, a second operation called a wide local excision is usually advised.
Wide local excision may be needed
This aims to remove an area of normal skin around where the melanoma had been (before it was removed with excisional biopsy). This aims to make sure that any cells which may have grown in the local area of skin have been removed. The amount of normal-looking skin removed varies - depending on the thickness of the melanoma (how deep it has spread into the skin) as reported from the biopsy. It may be 1-2 cm around where the melanoma had been. This operation may be done under local or general anaesthetic. In some cases, a skin graft may be needed to cover the wound.
Staging of melanoma
The aim of staging is to find out how much a cancer has grown and spread. Finding out the stage of the cancer helps doctors to advise on the best treatment options. It also gives a reasonable indication of outlook.
Most cases of melanoma are diagnosed at stage one when there is a very good chance that treatment will cure the condition. Other stages (2-4) are diagnosed if the tumour has spread. The stage diagnosed depends on how much and how far the original tumour has spread to other parts of the body.
How is melanoma assessed and staged?
If the initial biopsy and the tissue taken from the wide local excision show that the melanoma is just in the top layer of skin and is less than 0.76 mm thick then no further tests are usually needed. It is highly unlikely that it will have spread. This is an early stage 1 melanoma.
A doctor will examine you to see if you have any swollen lymph glands (nodes) near to the melanoma. If you have, the melanoma may have spread to these local lymph nodes.
It is possible that there may be some early spread without causing symptoms if the melanoma is thicker than 0.76 mm on the initial biopsy. In particular, there may be spread of some cells to the nearest lymph node without it yet causing it to swell. Therefore, a test called sentinel lymph node biopsy, and sometimes other tests, may be advised.
Sentinel lymph node biopsy
This is a relatively new test which may be considered. In this test, a small sample of the nearest lymph node is taken as an additional procedure when the melanoma is being removed. However, sentinel lymph node biopsy is not used routinely and is usually performed only as part of a research study. This means that it is not an essential part of treatment.
Other tests
Tests which may be advised depend on:
- Whether you have symptoms.
- Whether the lymph nodes are found to be involved.
- The thickness of the primary melanoma (the thicker the primary tumour, the greater the chance of spread).
The tests aim to detect if the cancer has spread to other parts of the body. For example, you may be advised to have X-rays, blood tests, scans, etc.
What is the treatment for melanoma?
The treatment depends on the stage. Generally, if the melanoma is thin then a small operation to cut out the tumour (the biopsy or wide local excision described above) is usually all the treatment that is needed. This is likely to clear all the cancer cells. Following the treatment, you will usually be seen at regular intervals.
If the melanoma is deeper then you may need a larger operation which may include removing the local lymph glands (nodes). You may also be given additional treatment, depending on where the cancer has spread to and what symptoms you have.
This may include:
- Chemotherapy: This is a treatment which uses anti-cancer medicines to kill cancer cells or to stop cancer cells from multiplying.
- Radiotherapy: This treatment uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells or stops the cells from multiplying.
- Immunotherapy: This aims to boost the immune system to help to fight cancer.
Prognosis
What is the outlook?
The outlook (prognosis) for people with malignant melanomas has been improving over a period of 25 years and people with melanomas now have amongst the best outlook for any cancer. Around three quarters of people who have a melanoma removed will have no further problems.
The outlook depends on the stage. Most cases of stage 1 melanoma are cured with a minor surgical operation to remove the tumour (described above). For people with deeper melanomas then there is still a chance of cure. People with advanced melanoma that has spread to other parts of the body are not likely to be cured. However, treatment can often slow down the progression of the cancer.
The treatment of cancer is a developing area of medicine. New treatments continue to be developed and the information on outlook above is very general. The specialist who knows your case can give more accurate information about your particular outlook and how well your type and stage of cancer are likely to respond to treatment.
Prevention
Can melanoma be prevented?
Most skin cancers (non-melanoma and melanoma skin cancers) are caused by excessive exposure to the sun.
We should all limit our sun exposure in the summer months (or all year when in hot countries nearer the equator) by:
- Staying indoors or in the shade as much as possible between 11 am and 3 pm.
- Covering up with clothes and a wide-brimmed hat when out in the sunshine.
- Applying sunscreen with a sun protection factor (SPF) of 15 (SPF 30 for children or people with pale skin) which also has high ultraviolet A (UVA) protection.
In particular, children should be protected from the sun. Sunburn or excessive exposure to the sun in childhood is thought to be the biggest risk factor to the developing of skin cancer as an adult. Also, people with a family history of melanoma should take extra care to protect their skin from the sun.
About the author
Dr Colin Tidy
MBBS, MRCGP, MRCP, DCH
Dr Colin Tidy qualified as a doctor in 1983 and he has been writing for Patient since 2004. Dr Tidy has 25 years’ experience as a General Practitioner. He now works as a GP in Oxfordshire, with a special interest in teaching doctors and nurses, as well as medical students. In addition to writing many leaflets and articles for Patient, Dr Tidy has also contributed to medical journals and written a number of educational articles for General Practitioner magazines.
Recommended websites
For further reading go to:
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
