Back Conditions Explained
Varicose Veins
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Laurence Knott (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
There are no accurate figures for the number of people with varicose veins. Some studies suggest that 3 in 100 people have them at some time in their lives. Most people with varicose veins do not have an underlying disease and they usually occur for no apparent reason.
Varicose veins do not cause symptoms or complications in most cases, although some people find them unsightly. If treatment is advised, or wanted for cosmetic reasons, a procedure to seal them off is used. There are several procedures available: heat, lasers or chemicals injected into the veins. These methods have largely replaced the old-fashioned surgical methods such as stripping the veins out.
Understanding normal leg veins
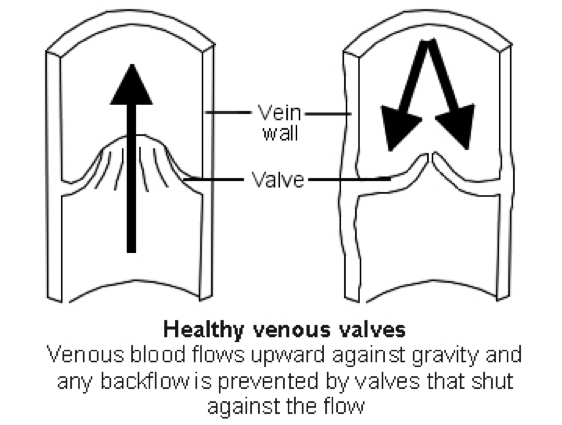
Veins are blood vessels which take blood back to the heart. Blood flows up the leg veins, into larger veins and towards the heart.
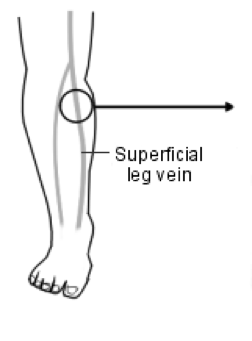
There are three types of veins in the legs:
- Superficial veins, which are the ones just below the skin surface. You can often see or feel the larger superficial veins. The superficial leg veins are the ones that may develop into varicose veins.
- Deep leg veins, which pass through the muscles. You cannot see or feel these.
- Many small communicating (perforator) veins, which take blood from the superficial veins into the deep veins.
There are one-way valves at intervals inside the larger veins. These valves prevent blood flowing back in the wrong direction. When we stand there is quite a height of blood between the heart and legs. Gravity tends to pull the blood back down but is prevented from doing so by the vein valves and by the normal flow of blood towards the heart.
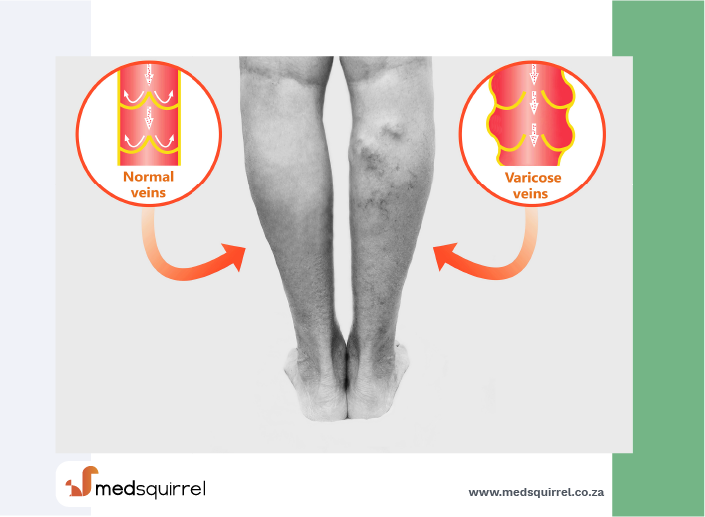
What are varicose veins?
Varicose veins are enlarged (dilated) sections of veins which are located just under the surface of the skin - usually on the leg. They are often easy to see, as they look thick and knobbly. They may be less obvious if you are overweight, as they are hidden by fatty tissue under the skin.
Other, smaller types of veins which can be noticeable are:
- Reticular veins: a closely grouped network of small veins.
- Thread veins, or spider veins: these look like a kind of star burst pattern on an area of the leg. They are not true varicose veins.
Causes
What causes varicose veins?
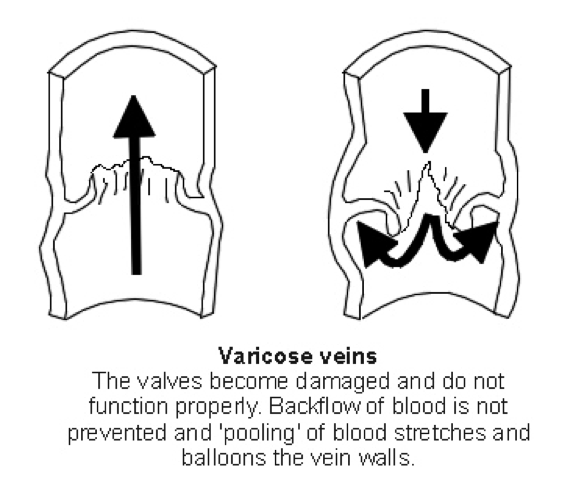
It is thought that the wall of the vein becomes weak in some sections. These sections then widen and become more prominent.
If this occurs near a valve, then the valve may become leaky and blood may flow backwards. Once this happens at one valve there is extra pressure on the vein. This can cause more widening and more leaky valves. Blood then pools (collects) in the enlarged vein and makes it stand out.
Who develops varicose veins?
About 3 in 100 adults develop varicose veins at some time in their lives. More women than men develop varicose veins. Most people with varicose veins do not have an underlying disease and they occur for no apparent reason.
However, the chance of them developing is increased with:
- Pregnancy: This is partly due to the baby causing extra pressure on the veins and partly because hormones you make during pregnancy tend to relax vein walls. The more babies you have, the more the risk of permanent varicose veins developing. Varicose veins tend to appear, or become worse, during pregnancy but often improve after childbirth when the pressure on the veins eases.
- Age: They are more common with increasing age.
- Being overweight: which appears to increase the chance for women but not for men.
- Standing a lot. Jobs which involve lots of standing are often said to cause varicose veins. However, there is little scientific evidence to support this theory.
- Sometimes an underlying disease may cause varicose veins - for example:
- A previous blood clot in leg (thrombosis)
- A previous injury to the deep veins in the leg.
- Rarely, a swelling or tumour in the lower part of the tummy (the pelvis) which blocks flow in the veins at the top of the leg.
- Very rarely, varicose veins are due to abnormal blood vessels - if some of the veins or arteries have not formed in the normal way.
Symptoms
What are the symptoms of varicose veins?
Most people with varicose veins have no symptoms. Some people are concerned about the appearance of the veins. Larger varicose veins can ache, feel heavy or itch.
Are there any complications of varicose veins?
Most people with varicose veins do not develop complications. Complications develop in a small number of cases. Complications are due to the higher pressure in the varicose veins causing changes to the small blood vessels in nearby skin.
If complications do develop, it is typically several years after the varicose veins first appear. However, it is impossible to predict who will develop complications. The visible size of the varicose veins is not related to whether complications will develop.
Possible complications include:
- Inflammation of the vein (thrombophlebitis).
- Swelling of the foot or lower leg.
- Skin changes over the prominent veins. The possible skin changes are discolouration, varicose skin ulcers, or “lipodermatosclerosis” - hardening of the fat layer under the skin, causing areas of thickened, red skin.
- Rarely, varicose veins may bleed.
First aid for bleeding varicose veins: bleeding happens only rarely. If a varicose vein does bleed then you need to stop the bleeding quickly by doing the following:
- Raise the leg: lie down flat and raise the leg high. This will ensure that it is well above the rest of the body (for example, rest it on a chair, use lots of pillows or someone can hold the leg high).
- Pressure: put a clean cloth or dressing on to the bleeding area and put firm pressure on it, for at least 10 minutes.
- Call an ambulance if the bleeding is heavy or does not quickly stop. See a doctor urgently, as you may need treatment to prevent the bleeding from happening again.
Treatment
Do I need treatment or a referral for varicose veins?
Most people with varicose veins do not need any treatment.
You may want to have treatment for one of the following reasons:
- If complications develop: these occur in a small number of cases. If leg swelling or skin changes develop over prominent veins, treatment is usually advised to prevent a skin ulcer from developing. If a skin ulcer does occur, then treatment of any varicose veins may help to cure the ulcer. If you have a varicose vein which has bled, you should be referred urgently for treatment.
- For symptoms of itch or discomfort.
- Cosmetic reasons: You may feel that the veins look unsightly. Treatment which is purely for cosmetic reasons is not usually usually paid for by medical funders.
Combination symptoms:
you will need to have the leg circulation examined before certain treatments (such as compression stockings) can be used if you have a combination of BOTH:
- Varicose veins which are problematic; AND
- Arterial disease (poor circulation, or peripheral arterial disease) of the legs.
Which tests might I have?
If varicose veins are problematic, you will usually be referred for assessment by a doctor who is a specialist. You may have a type of ultrasound scan called a Doppler or a duplex scan. This helps to show how the blood is flowing in the veins. It can show whether any of the valves are damaged - which is useful to know when planning treatment. Occasionally, other tests are needed if the veins are complex.
If you have arterial disease (poor circulation, or peripheral arterial disease) in your legs, or if arterial disease is suspected, the arterial circulation needs to be measured. This needs to be done before you have treatment which puts pressure on the leg, such as compression stockings (below). The arterial circulation is normally measured by using an ultrasound machine called a Doppler ultrasound, which is used to give a measurement called the ankle brachial pressure index. This test can be done in specialised clinics and also by some nurses and GPs.
What are the treatment options for varicose veins?
There are several different options. Traditional operations such as vein stripping have largely been replaced by procedures which involve heat, lasers or the injection of chemicals into the vein.
Self-help methods:
- Avoid prolonged standing or sitting still. Try to put your feet up frequently (sit or lie down and raise the feet above the level of your hips). You can, for example, use extra pillows under your feet on a bed or footrest). This helps to reduce blood pooling in the veins. Use a moisturising cream or ointment to protect the skin in the affected area if it is dry, flaky or itchy.
- Weight loss and exercise are unlikely to make varicose veins disappear but may prevent them from developing in the first place.
Varicose vein treatment techniques have been developed which have a lower rate of complications, such as bruising, compared with traditional surgery. The National Institute for Health and Care Excellence (NICE) recommends that they be used in preference to traditional surgery for people who are having their veins treated for the first time. They include:
- Radiofrequency ablation and endovenous laser ablation: These methods involve passing a probe into one of the longer varicose veins, using ultrasound to guide the position. The laser or radiofrequency energy makes the vein heat up, which seals it.
- Foam sclerotherapy: This technique is used if heat or lasers do not work. It uses a chemical mixed with air to make foam. The foam is injected into the veins, pushing the blood away and making the veins go into spasm. After treatment, compression stockings are needed, and the veins will be hard and swollen for a while before they shrink down. More than one treatment may be needed
Surgery: Traditional surgery is recommended if treatment with heat, lasers or foam does not work. Different techniques can be used to remove the veins, depending on their site and severity. A surgeon will advise. Usually, the communicating veins (explained above) are tied off (ligated). Then the large varicose veins are removed or stripped from the leg. Many people can be treated as day cases. One to three weeks off work may be needed afterwards, depending on your job.
Sclerotherapy: The vein is injected with a chemical that can close and seal (sclerose) it. It was once used as a main treatment, but it became clear that it commonly causes skin staining and ulcers. It is now mainly reserved for small veins below the knee which have not been treated properly or have come back after surgery. The vein needs to be compressed afterwards, which involves wearing bandaging or compression stockings for a few days or weeks.
Support tights and compression stockings: These counter the extra pressure in the veins. They may help to ease symptoms such as ache, although there is little proof as to how well they work. They may be difficult to put on, particularly by people who have arthritis in their hands. Current guidelines do not recommend that they be used routinely unless treatments to seal the veins are not suitable or do not work. If you do need compression stockings, below-knee class 1 (light) or class 2 (medium) are usually the most suitable. Ideally, they should be put on first thing in the morning, before you get out of bed, then taken off when going to bed at night. Compression stockings are available on prescription or you can buy them.
Note: if you have arterial disease in the legs, you will need a medical assessment of your circulation to decide if compression stockings are suitable (see above).
Thread veins and spider veins
These do not cause the same problems as varicose veins, and do not need treating except for cosmetic reasons.
About the author
Dr Laurence Knott
BSc (Hons) (Biochemistry), MB BS
Qualified 1973. 37 years experience in general practice. Medical author who has contributed to many lay and professional publications. Particularly interested in converting medical terminology into information comprehensive to non-medical readers. Clinical complaints adviser to the Medical Defence Union. External professional adviser to the Health Service Ombudsman. Extensive medicolegal practice specialising in clinical negligence. Listed on the National Crime Database, advising police forces and the Crown Prosecution Service on medicolegal aspects of criminal cases. Erstwhile GP medical adviser to the Guillain-Barré & Associated Inflammatory Neuropathies charity, now member and ex-patient.
Recommended websites
For further reading go to:
- Varicose Eczema - A skin condition that mainly occurs in the elderly
- Venous Leg Ulcers - Common in older people
- Superficial Thrombophlebitis - Inflammation of a vein just under the skin
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
