Back Conditions Explained
Yeast Infection in Women
Also known as "Vaginal Thrush"

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Mary Harding (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Vaginal thrush is an infection of the vagina and/or vulva with a yeast germ called candida. We all have millions of germs living inside us all the time. Some of these germs are actually helpful to us - for instance, 'friendly' bacteria in the gut help us to digest our food. Many others don't cause any harm, or any symptoms, unless they multiply too much.One of these germs is a type of fungus, a family of yeasts called Candida spp. Fungi like warm, moist, airless places, and a vagina is a perfect home for them. Small numbers of Candida spp. commonly live on the skin and around the vaginal area. Most of the time, they don't cause any problems. However sometimes they multiply and cause symptoms.
Candida albicans, a fungus that often causes oral and genital infections in humans
Image credit: obtained from the website std-gov.org
Who gets thrush?
Up to three quarters of all women will have at least one bout of thrush in their lives. In most cases it develops for no apparent reason. However, certain factors can make thrush more likely to develop. The vagina contains mucus and some harmless bacteria which help to defend the vagina from candidal infection (and other germs).
These natural defences may be altered or upset by certain situations:
- When you are pregnant.
- If you have diabetes.
- If you take antibiotic medication.
- If your immune system is not working normally. For example, if you are on chemotherapy for certain cancers, if you are taking high-dose steroids, etc.
So, in these situations you may be more likely to develop thrush. You may also be more prone to recurring episodes (recurrent thrush) although some women develop repeated episodes of thrush with no obvious triggers.
There is some relationship between thrush and the female hormone oestrogen. Thrush is much more common in the "reproductive years", i.e. the years between starting to have periods and stopping for menopause when it is possible to have a baby. Some women are prone to thrush in certain times of their menstrual cycle - for example, before a period. The hormone changes of pregnancy make thrush more likely. It may be that hormone pills such as hormone replacement therapy (HRT) and the combined oral contraceptive (COC) pill make you more prone to thrush. This is not yet certain, however.
Causes
What causes vaginal thrush?
Thrush is not considered to be a sexually transmitted infection, although occasionally it is passed on during sex. More often it is an overgrowth of the Candida yeast which is already there but not previously causing a problem.
The immune system and the harmless germs (bacteria) that also normally live on the skin and in the vagina usually stop Candida spp. from thriving. However, when conditions are good for Candida spp., numbers multiply and may invade the vagina and cause symptoms. This could be due to changes in the bacteria in the vagina when you have taken antibiotics. Or it could be related to hormone changes, or problems with your immune system.
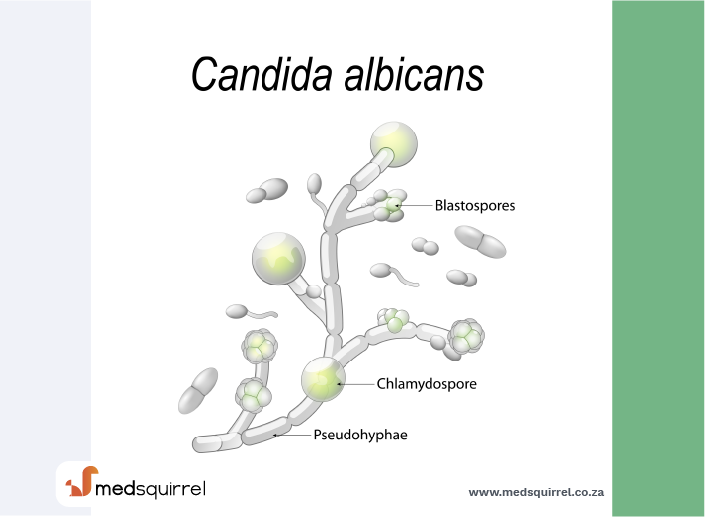
Most causes of thrush are a result of Candida albicans, but sometimes other types of Candida spp. such as Candida glabrata or Candida tropicalis are the cause.
Symptoms
What are the symptoms of vaginal thrush?
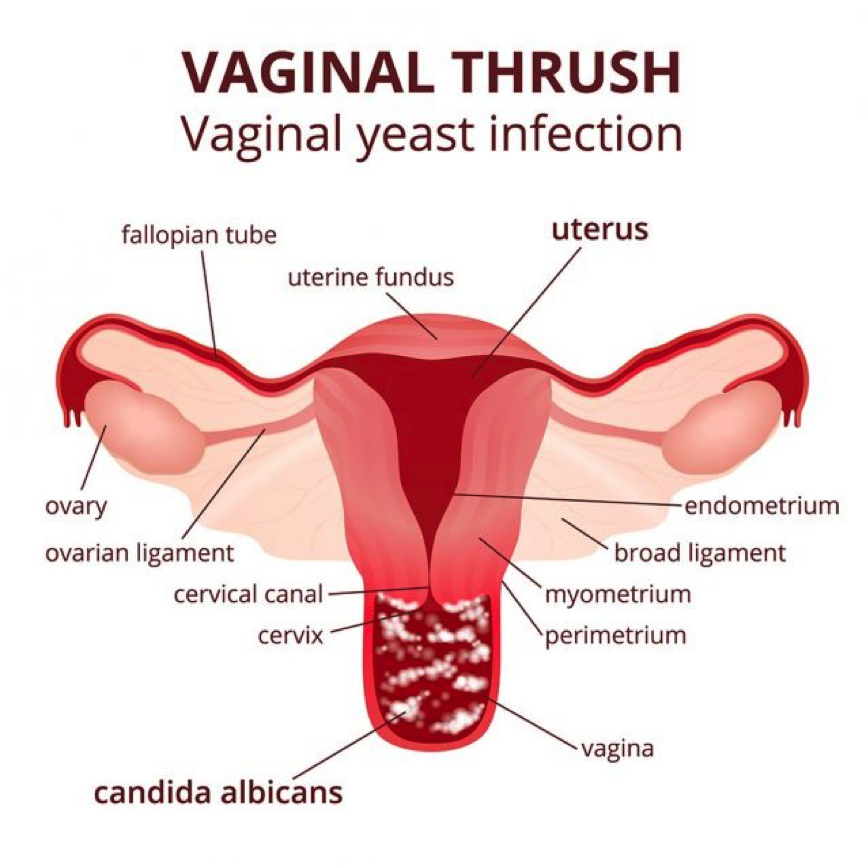
Itch of the skin folds outside the vagina (the vulva) is the most common symptom of thrush. It may be itchy inside the vagina also.
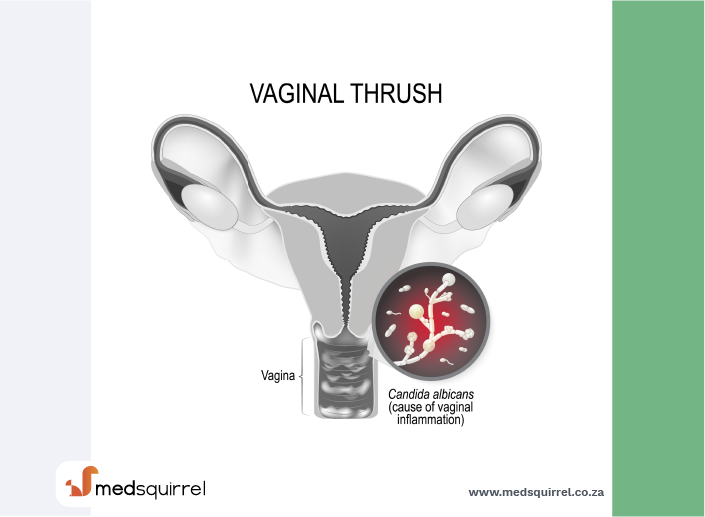
The female reproductive system during vaginal yeast infection
Image credit: obtained from the website std-gov.org
How would I know if I have a yeast infection?
There may also be soreness of the vulva: Sometimes it may be painful to pass urine and/or painful to have sex. If there is soreness without itching, this is more likely to have another cause.
There may also be a discharge from the vagina: Thrush is the second most common cause of a vaginal discharge. (The most common cause of vaginal discharge is bacterial vaginosis).
The discharge from thrush is usually creamy white and quite thick but is sometimes watery. It can add to the itch, redness, discomfort, or pain around the vulva. The discharge from thrush does not usually smell.
Sometimes symptoms are minor and clear up on their own. Often symptoms can be quite irritating and will not go without treatment.
Symptoms that suggest thrush is severe include:
- Redness (erythema) - usually around the vagina and vulva but may extend to the labia majora and perineum.
- Vaginal fissuring and/or swelling.
- Scratch marks (excoriation) on the vulva.
- Other skin rashes near to the vagina (called satellite lesions) - this is rare and may indicate other fungal conditions or herpes simplex virus.
Thrush does not damage the vagina and it does not spread to damage the womb (uterus). If you are pregnant, thrush will not harm your baby.
Symptoms which suggest your symptoms ARE NOT due to thrush include:
- A smelly or coloured discharge.
- Bleeding between periods or after having sex.
- Needing to pass urine more often.
- A rash or blisters on the skin of the vulva.
Diagnosis
How is vaginal thrush diagnosed?
You do not always need a test to diagnose thrush. The diagnosis is often based on the typical symptoms and signs.
It is important that you do not assume that a vaginal discharge is thrush. There are other causes of vaginal discharge.
It is reasonable to assume it is thrush if:
- You have a vaginal and/or vulval itch.
- Any discharge you have does not smell and is white or creamy.
- You have no abnormal bleeding.
However, if you have assumed you have thrush and you have had treatment, but the symptoms have not gone away, you may need to have tests. See your doctor, who may examine you and may perform some tests.
If tests are needed they may include:
Over-the-counter test: A test to see how acidic the vagina is (a pH test). The level of acidity gives an indication of whether a discharge is due to thrush or to bacterial vaginosis. This is the basis of the over-the-counter test for thrush. A test strip is placed into the vagina and then the colour change indicates if thrush is likely or not. A pH level of 4.5 or less suggests thrush. Some doctors may also use this test.
A swab: This is a stick with a cotton bud at the end of it. A sample of discharge is taken from the vagina and analysed in a lab. This indicates if you have thrush or another infection. It can also inform the doctor which type of candida you have.
Tests for other infections: Further swabs may be taken to be sure you do not have other types of vaginal infections.
Urine tests: Your urine may be checked for sugar. This is to check you do not have diabetes, as this would make you more prone to thrush. This might be done if you were getting repeated (recurring) episodes of thrush. Urine may also be checked for infection, as sometimes it can be difficult to distinguish between a urine infection and thrush.
A colony of Candida growing in Petri dish
Image credit: obtained from the website std-gov.org

Do I need to see a doctor if I get vaginal thrush?
If you have had thrush in the past and the same symptoms come back, then it is common practice to treat it without an examination or tests. Many women know when they have thrush and treat it themselves. You can buy effective treatments without a prescription from pharmacies.
However, remember a vaginal discharge or vulval itch can be due to a number of causes. So, do not assume all discharges or itches are thrush.
The following gives a guide as to when it may be best to see a doctor or nurse if you think that you might have thrush. If you:
- Are under 16 or over 60 years of age.
- Are pregnant.
- Have treated yourself with a thrush treatment from the chemist, but your symptoms have not gone away.
- Have abnormal vaginal bleeding.
- Have lower tummy (abdominal) pain.
- Are unwell in yourself in addition to the vaginal and vulval symptoms.
- Have symptoms that are not entirely the same as a previous bout of thrush. For example, if the discharge has a bad smell, or it you develop ulcers or blisters next to your vagina.
- Have had two episodes of thrush in six months and have not consulted a doctor or nurse about this for more than a year.
- Have had a previous sexually transmitted infection (or your partner has).
- Have had a previous bad reaction to anti-thrush medication or treatments.
- Have a weakened immune system - for example, if you are on chemotherapy treatment for cancer or are taking long-term steroid medication for whatever reason.
And if you do treat yourself, see a doctor or nurse if the symptoms do not clear after treatment.
Treatment
What are the treatments for vaginal thrush?
There are a few different options for treating thrush. Some are applied directly to the vagina and/or vulva; others are medicines which are swallowed orally.
Topical thrush treatments
These are pessaries and creams which you insert into the vagina with an applicator. They contain anti-yeast medicines such as clotrimazole, econazole or miconazole. A single large dose inserted into the vagina is often sufficient to clear a bout of thrush. Alternatively, a lower dose is used for several days. You may also want to rub some anti-thrush cream on to the skin around the vagina (the vulva) for a few days, especially if it is itchy. In mild cases, or for girls under the age of 16, a cream for the skin may be all that is needed.
You can obtain topical treatments on prescription, or you can buy some of them without a prescription at pharmacies. Side-effects are uncommon, but read the information leaflet that comes with the treatment for full information.
In general, you can use these topical treatments if you are pregnant, but you should always check with your doctor or pharmacist. Treatment is usually needed for longer during pregnancy.
Note: some pessaries and creams may damage latex condoms and diaphragms and affect their use as a contraceptive. You should use alternative methods of contraception during treatment and for several days afterwards.
Tablets
Two options are available:
- Fluconazole, which is taken as a single dose
- Itraconazole, which is taken as two doses over the course of one day. You can obtain these treatments on prescription; you can also buy fluconazole without a prescription from pharmacies. Side-effects are uncommon, but always read the information leaflet that comes with the treatment for full information. Do not take these treatments if you are pregnant or breast-feeding. You may also want to rub some anti-yeast cream on to the skin around the vagina for a few days, especially if it is itchy. Combination packs containing both the tablet and the cream are available. In severe infection, a repeat dose of the tablet may be suggested after three days.
Note: tablets and topical treatments are thought to be equally effective. Tablets are more convenient but are more expensive than most topical treatments.
If you are in a sexual relationship, there is NO NEED to treat your partner too unless they also have symptoms.
Image credit: obtained from the website std-gov.org

Other things that may help
If you have thrush, you may also find the following things help to relieve your symptoms:
- Avoiding wearing tight-fitting clothing, especially clothing made from synthetic materials. Loose-fitting, natural-fibre underwear may be better.
- Avoiding washing underwear with biological washing powders or liquids and avoiding the use of fabric conditioners.
- Avoiding using perfumed products around the vaginal area, such as soaps and shower gels, as these may cause further irritation.
- Using a simple emollient every day as a moisturiser to protect the skin around the vulva.
- Yoghurt containing probiotics, either eaten or applied to the vagina, may be helpful; however, there is not yet enough evidence to know if it is proven to be effective.
What if the treatment doesn't work?
If you still have symptoms a week after starting treatment, then see your doctor. Treatment does not clear symptoms in up to 1 in 5 cases.
Reasons why treatment may fail include:
- The symptoms may not be due to thrush: There are other causes of a vaginal discharge. Also, thrush can occur at the same time as another infection. You may need tests such as vaginal swabs (samples taken using a small ball of cotton wool on the end of a thin stick) to clarify the cause of the symptoms.
- Most bouts of thrush are caused by C. albicans. However, about 1 in 10 bouts of thrush are caused by other strains of Candida spp., such as C. glabrata. These may not be so easily treated with the usual anti-thrush medicines.
- You may not have used the treatment correctly.
- You may have had a quick recurrence of a new thrush infection. (This is more likely if you are taking antibiotic medication, or if you have undiagnosed or poorly controlled diabetes).
Prevention
How do you prevent vaginal thrush?
These tips may help you to avoid thrush, or avoid it coming back. However, they have not been proven to work by research. Their use is based on common practice rather than research studies:
- Hygeine: Thrush IS NOT due to poor hygiene. However, the normal conditions of the vagina may be altered by excess washing and rinsing out (douching) of the vagina, bubble baths, scented soaps, spermicides, etc. The normal mucus and germs (bacteria) in the vagina may be upset by these things and allow Candida spp. to infect. Therefore, it may be best to wash just with water and unscented soap and not to douche the vagina.
- Clothes: Don't wear nylon underwear or tight-fitting jeans too often. Loose cotton pants are best. Stockings rather than tights are preferable. The aim is to prevent the vaginal area from being constantly warm, moist and airless. Avoid washing underwear in biological washing powder and using fabric conditioners.
- Antibiotic medicines: Be aware that thrush is more likely if you take antibiotics for other conditions. Antibiotics may kill the normal harmless bacteria in the vagina which help to defend against Candida spp. As Candida spp. are yeasts and not bacteria, they will not be killed by antibiotics. This is not to say that every course of antibiotics will lead to thrush. But, if you are prone to this problem and you are prescribed antibiotics then have some anti-thrush treatment ready to use at the first sign of thrush.
- Sex: Thrush is not a sexually transmitted infection. However, friction when you have sex may cause minor damage to the vagina which may make Candida spp. more likely to thrive. So, make sure your vagina is well lubricated when having sex. If natural secretions are not sufficient then use a lubricant when you have sex. After sex, wipe yourself so you are clean and dry.
It may also be worth reviewing any medication you are taking, as some medicines can make you more prone to thrush. You should discuss this with your doctor.
About the author
Dr Mary Harding
BA, MA, MB BChir, MRCGP, DFFP
Mary qualified at Cambridge in 1989. She joined EMIS as an author in 2013. Mary is a part-time, salaried GP at The Village Surgery, Wheathampstead and previously for 12 years in Welwyn Garden City. Mary is also an appraiser and Senior Appraiser for NHS England, in the Central Midlands area team.
Recommended websites
For further reading go to:
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
