Back First Aid Explained
How to Treat Sudden Cardiac Arrest

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website wikiHow. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Sudden cardiac arrest is the leading cause of death among adults over the age of 40 in the United States and other countries. About as many people die each year from SCA as die from Alzheimer's disease, assault with firearms, breast cancer, cervical cancer, colorectal cancer, diabetes, HIV, house fires, motor vehicle accidents, prostate cancer and suicides combined. However, with cardiopulmonary resuscitation (CPR) and the use of an AED, survival rates increase to 38%. Learn how to treat sudden cardiac arrest so that you will know what to do in an emergency.
Part 1: Detecting Sudden Cardiac Arrest
1. Watch for a sudden collapse or fainting
Someone who has just experienced cardiac arrest may lose consciousness and fall to the ground without warning. If you notice someone collapse or faint, go over to the person right away.

2. Check for a pulse
If someone has just had sudden cardiac arrest, then that person will not have a pulse. Check the person’s radial or carotid pulse to see if you can detect anything.
- The radial pulse is located on your wrist just under the base of the thumb/palm. Feel around the person’s wrist, using your index (first finger) and middle finger on one hand until you find the pulse. If you can't feel a beating pattern than there is no pulse.
- The carotid pulse is located on the neck. The carotid arteries are just underneath the jaw on both sides of the neck. Press the same two fingers on one side of the neck in the soft hollow area just beside the person’s Adam’s apple.

3. See if the person is beathing
A person who has experienced a sudden cardiac arrest will also not be breathing. "Look, listen, and feel" if the person is breathing or not. Watch for lung movement to determine if the person is getting any oxygen. Keep in mind that time is critical and every minute that the person is without oxygen increases his risk of permanent brain damage.
- Place your hands, palms down, on the person’s chest. Then, check to see if you can feel or see a rise and fall of the chest indicating breathing. An alternative method is to listen for breathing by placing your ear close to the person’s mouth.

4. Determine if the person is alert
A person who has had sudden cardiac arrest will not be alert either. This means that if you say something to the person, she will not respond or make any sign that she has heard you.
- Medical practitioners and first-responce assistants suggest using the C.O.W.S system: Can you hear me? Open your eyes! What's your name? Squease my hand (gently place your hand on their palm)!

Part 2: Administering Basic Life Support
1. Tell someone to call emergency services or call yourself if no one else is around
(See "EMERGENCY NUMBERS" above)
This should be your first priority. Someone who has suffered sudden cardiac arrest will need immediate medical attention and will need to be taken to a hospital for the best chances of survival. Make sure that you call for help right away or have someone else do so.
- Do not just shout for anyone to call 10177. If there are other people around, select one person, look him in the eye, and tell him to contact emergency services. Say something like, "You, the man in the red shirt! Call 10177 now!"

2. Locate an AED
If you are somewhere that might have a public AED (cardiac defibrillator), ask someone to try to locate it and bring it to you. If one is available right away, then use it. An AED can analyze the heart rhythm, deliver life-saving shocks, and provide instructions as well as images to help you revive the person.

3. Check for breathing and a pulse again
Quickly check the unconscious person’s pulse and breathing again to see if she has resumed breathing or if you can detect a pulse. If not, then you will need to start CPR.
- Cardiopulmonary resuscitation allows manual compression of the heart to pump blood and manual assisted breathing to get oxygen to the person. Those who have no pulse and/or are not able to breath on their own require immediate CPR.

4. Position the victim
Make sure the person is lying face up. You will need to be able to press on the person’s chest and deliver breaths, so turn the person over if he is not lying face up.
- If you suspect head and/or neck injury, do not move the person. This may result in paralysis or other serious complications. Provide as much aid as you can without moving the person.

5. Get yourself into position
Before you start delivering CPR, take a moment to make sure that you are in the right position. Place the heel of one of your hands on the center of the chest over the lower part of the bony center (breastbone). Place the heel of the other hand over top on the first hand. Straighten your arms and make sure your shoulders are directly over your hands.

6. Begin compressions
Once you are in position, you can begin compressions. Push down hard and fast. Your compressions should press down a minimum of two inches on the chest and allow for full chest recoil as well.
- Your pace should be such that you are delivering about 100 compressions per minute. An easy way to keep this pace is to deliver compressions to the beat of the song "Stayin' Alive."

7. Deliver two breaths of air after every 30 compressions
You should count your compressions so that you know when to deliver the two breaths. Before delivering the two breaths, tilt the person’s head by back slightly by placing the palm of one hand on the forehead and using your other hand to lift the chin. Once the head is tilted, pinch the person’s nose, cover the person's mouth with yours, and blow until you see the chest rise. Give the person two breaths. Each breath should take one second to deliver.
- After completing 30 compressions, deliver the two breaths and then deliver 30 more compressions. Keep repeating the cycle until help or an AED arrives.
- If you are not certified in CPR, you can skip the breaths. The emphasis for a bystander is on delivering chest compressions.
- CPR is exhausting and can be intense (you may break the person's ribs while delivering compressions). It's okay to trade off with someone else if you become exhausted — it doesn't help if you are too tired to deliver CRP properly.
- If you suspect head or neck trauma it is best not to perform the tilt technique, instead a jaw thrust should be performed so as not to aggravate the neck. Place the palms of your hand over the person’s cheek bone and place fingers under the angle of the jaw and lift the jaw upward.

Part 3: Using an Automated External Defibrillator
1. Understand what an Automated external defibrillator (AED) does
The heart pumps blood or beats due to an internal electrical system. This allows the heart to beat at a constant rhythm. When this system malfunctions or stops, the heart stops beating or beats irregularly losing its rhythm. An AED is a portable device that checks the heart rhythm and can send an electric shock to the heart to try to restore a normal rhythm if necessary.
- If an AED is available, then use it immediately! If it is not available, then continue CPR until it is or until help arrives.
- It is safe to use an AED on a pregnant woman. Defibrillation does not transfer any significant electrical current to a fetus.
- The AED machine only delivers a shock once it has analyzed the heart rhythm and determines if it is needed. If so, it will prompt everyone to stand clear of the person receiving the shock and not to touch them. However, you should still screen to make sure no one is in contact with the person before pressing the “shock” button by yelling "Clear!"

2. Find someone who knows how to use an AED if possible
A defibrillator works best when used by someone with proper training. In situations where lots of people are around, ask if anyone knows how to use a defibrillator. If no one is available, do not panic. The machine gives directions and voice prompts once it has been turned on, so that anyone can use it.

3. Check for puddles or water near the person
Water conducts electricity, so it is a bad idea to use an AED in wet conditions. You may end up shocking yourself and others as well as the victim. If you notice that the person is lying in or near a puddle, then move the person to a dry area before using the AED.

4. Turn on the AED and follow the instructions it gives
Although having some training in how to use an AED is ideal, the device will give you step-by-step instructions on how to use it. You'll hear voice prompts and/or see prompts on a screen. Follow the instructions carefully.
- A emergency operator may also be able to help guide you as you use the device. If you are not sure how to work the AED and no one else is around, call emergency services and ask for guidance (see "EMERGENCY NUMBERS" above).

5. Expose the person's chest and attach the sensors
If the person's chest is wet, dry it off. AEDs have sticky pads with sensors called electrodes. Apply the pads to the person's chest as pictured/described in the instructions or as described by the voice instructions.
- Place one pad on the right center of the person's chest above the nipple.
- Place the other pad slightly below the other nipple and to the left of the rib cage.

6. Press the AED's "analyze" button
The “analyze” button will check to see if the person has a pulse. Before you press the button, make sure no one is touching the person. Stay clear and instruct others to do the same while the machine checks the person's heart rhythm.

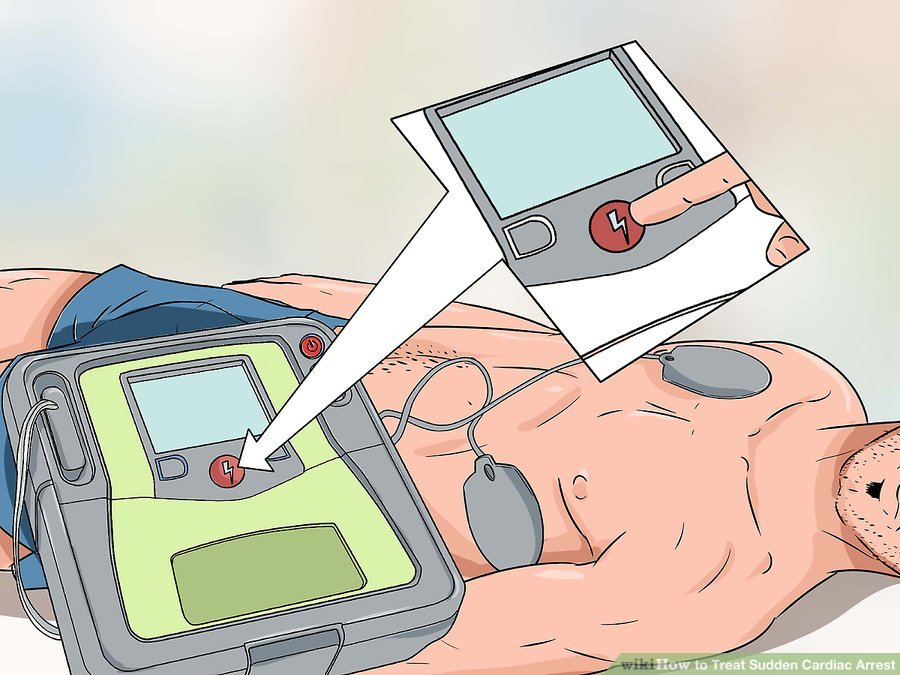
7. Deliver a shock when the machine instructs you to
If a shock is needed, the AED will let you know when to deliver it. Before you push the AED's "shock" button, stand clear of the person and make sure that others are clear as well.
8. Resume CPR after the shock has been delivered
After a shock has been delivered by the AED, resume CPR for two minutes. Give 30 compressions followed by two breaths. After two minutes of CPR check the neck artery for a pulse. If no pulse is present, press the “analyze” button to analyze the heart rhythm again and if a shock is advised deliver shock by pressing the “shock” button.
- Repeat this process until help arrives or pulse returns.

_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
