Back First Aid Explained
How to Do CPR on a Child


We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient wikiHow. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Though CPR (cardiopulmonary resuscitation) should be administered by individuals trained at a certified first aid course, lay bystanders can also make a significant difference in the survival of children undergoing cardiac arrest. For youth under one years of age, follow infant CPR protocol and for adults, follow adult protocol. Basic CPR involves chest compressions, airway opening and rescue breathing. If you are not formally trained in CPR, it is recommended that you use compression-only.
Part 1: Assessing the Situation
1. Check the scene for danger
If you come across someone who is unconscious, you need to quickly make sure there are no dangers to yourself if you choose to help them. Is there a car exhaust running? A gas stove? Is there a fire? Are electrical lines down? If there is anything that could endanger you or the victim, see if there is something you can do to counteract it. Open a window, turn off the stove, or put out the fire if possible.
- However, if there is nothing you can do to counteract the danger, move the victim. The best way to move the victim is by placing a blanket or a coat underneath her back and pulling on the coat or blanket.
- If there is a chance the person has suffered a spinal injury two people should move her to prevent any twisting of the head and neck
2. Check the victim for consciousness
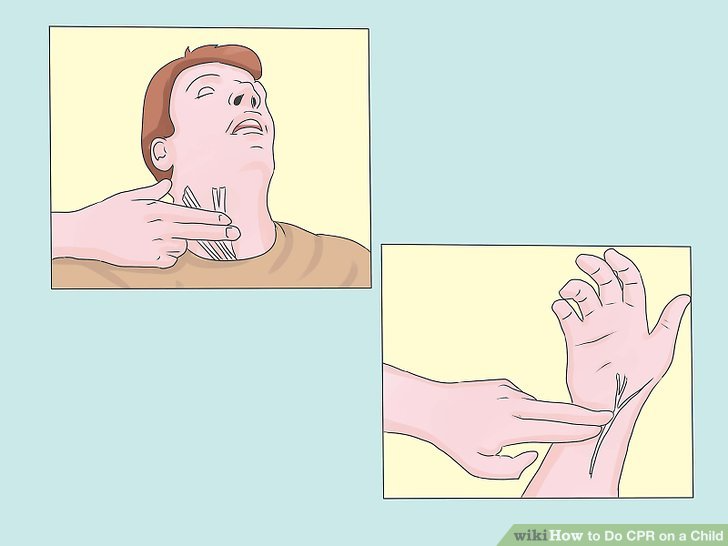
3. Check the victim's pulse
- To check the neck (carotid) pulse, feel for a pulse on the side of the victim's neck closest to you by placing the tips of your first two fingers beside the Adam's apple. (Be aware that the Adam's apple is usually not visible on a female, and may not even be very visible on a boy who has not yet gone through puberty).
- To check the wrist (radial) pulse, place your first two fingers on the thumb side of the victim's wrist.
- Other pulse locations are the groin and ankle. To check the groin (femoral) pulse, press the tips of two fingers into the middle of the groin. To check the ankle (posterior tibial) pulse, place your first two fingers on the inside of the ankle.
4. Understand the importance of reacting quickly
If you see someone whose heart has stopped beating or has stopped breathing, reacting quickly and performing rescue breathing and CPR could save his life. When someone starts CPR before an ambulance arrives, the patient has a considerably better chance of surviving. Being able to respond quickly by performing CPR, which can help get oxygenated blood back flowing to the brain, is essential.
- If the person has a pulse but is not breathing, only perform rescue breathing, not chest compressions.
- A human brain can typically go for around four minutes without oxygen before suffering permanent brain damage.
- If the brain goes without oxygen for between four and six minutes the chances of brain damage rise.
- If the brain lacks oxygen for six to eight minutes brain damage is probable.
- If the brain is without oxygen for over ten minutes, brain death is probable

Part 2: Performing CPR
1. Perform CPR for two minutes
- If someone else is there send them for help. If you are alone, do not call until you have completed two minutes of CPR.
- Dial your local emergency number: Call 10177 for an AMBULANCE. (See "EMERGENCY NUMBERS" above).
- If possible, send someone else to get an AED (Automatic External Defibrillator) if there is one in the building or nearby.
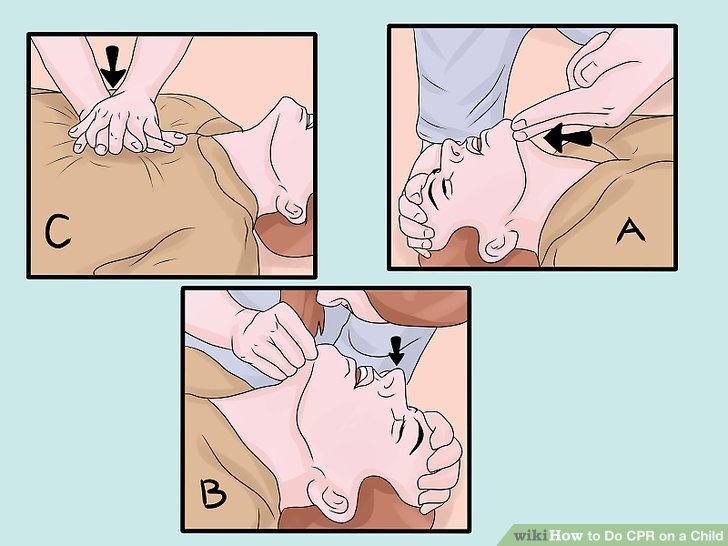
2. Remember CAB
In 2010, the recommended sequence changed with chest compressions placed before airway opening and rescue breathing. Chest compressions are more critical for correcting abnormal heart rhythms (ventricular fibrillation or pulseless ventricular tachycardia), and because one cycle of 30 chest compressions only requires 18 seconds, airway opening and rescue breathing are not significantly delayed.
- Chest compressions, or hands-only CPR is recommended if you have not been properly trained or are worried about performing mouth-to-mouth resuscitation on a stranger.
3. Position your hands for the compressions
When performing CPR on a child the positioning of your hands is especially important, given that a child will be more fragile than an adult. Locate the child's sternum by moving two fingers to the bottom of the rib cage. Identify where the lower the ribs meet in the middle and then place the heel of your other hand on top of your fingers. Just use the heel of this hand to do the compressions.
4. Perform 30 compressions
Compress the chest, with elbows locked, by pushing straight down about 2 inches (5.1 cm) deep. The smaller body of a child needs less pressure than an adult would. If you begin to hear or feel a cracking sound, that may indicate that you are pushing too hard. Continue, but apply less pressure with the compressions. Do 30 of these compressions, and do them at a rate of at least 100 compressions per minute if you are the only rescuer.
- Allow complete chest recoil after each compression.
- Minimize pauses in chest compression that occur when changing providers or preparing for a shock. Attempt to limit interruptions to less than 10 seconds.
- If there are two rescuers, each should complete a round of 15 compressions.
5. Make sure the airway is open
Place your hand on the victim's forehead and two fingers on his chin. Lift the chin gently with the two fingers while carefully pushing down on the forehead with your other hand. If you suspect a neck injury, gently pull the jaw upward rather than lifting the chin. Once you have done this you should look, listen and feel for breathing.
- Put your ear close to the victim's mouth and nose and listen carefully for any signs of life.
- Watch for chest movement and feel for any breath on your cheek.
- If there are no signs of life, place a breathing barrier (if available) over the victim's mouth.
6. Give two rescue breaths
Keeping the airway open, take the fingers that were on the forehead and pinch the victim's nose closed. Make a seal with your mouth over the victim's mouth and breathe out for about one second. Make sure you breathe slowly, as this will make sure the air goes in the lungs not the stomach. Make sure you keep your eye on the victim's chest.
- If the breath goes in, you should see the chest slightly rise and also feel it go in. If the breath goes in, give a second rescue breath.
- If the breath does not go in, reposition the head and try again. If it does not go in again, the victim may be choking. You'll need to do more chest compressions in this case. Keep in mind abdominal thrusts (the Heimlich manuever) should only be performed on someone who is conscious.
7. Repeat the cycle of 30 chest compressions and two breaths
You should do CPR for two minutes (five cycles of compressions to breaths) before checking for signs of life, a pulse or breathing. Continue CPR until someone takes over for you; emergency personnel arrive; you are too exhausted to continue; an AED is attached, charged, and the person running it asks you to clear the body; or pulse and breathing return.
- Don't forget to call the emergency services after the first two minutes of CPR.
- After you call them, continue to administer CPR until they arrive.
8. Use an AED
If an AED becomes available, turn on the AED, place the pads as instructed (one over the right chest and another over the left side). Allow the AED to analyse the rhythm, and give one shock if indicated, after clearing everyone from the patient (yell "CLEAR!" first). Resume chest compressions immediately after each shock for another 5 cycles before reassessing.
- If the victim begins breathing, gently manoeuvre them into the recovery position.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.