Back First Aid Explained
How to Check For a Fracture when Performing First Aid

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website wikiHow. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
Assessing an emergency situation that requires first aid can be stressful and difficult, especially when you're looking for or trying to assess injuries underneath the skin. Most emergency situations you're likely to encounter involve some sort of trauma, such as a fall, car accident or physical altercation. As such, checking for signs of a broken bone while administering basic first aid is important because it can help you stabilize the area and prepare the person for trained medical attention.
Part 1: Identifying Signs of a Bone Fracture
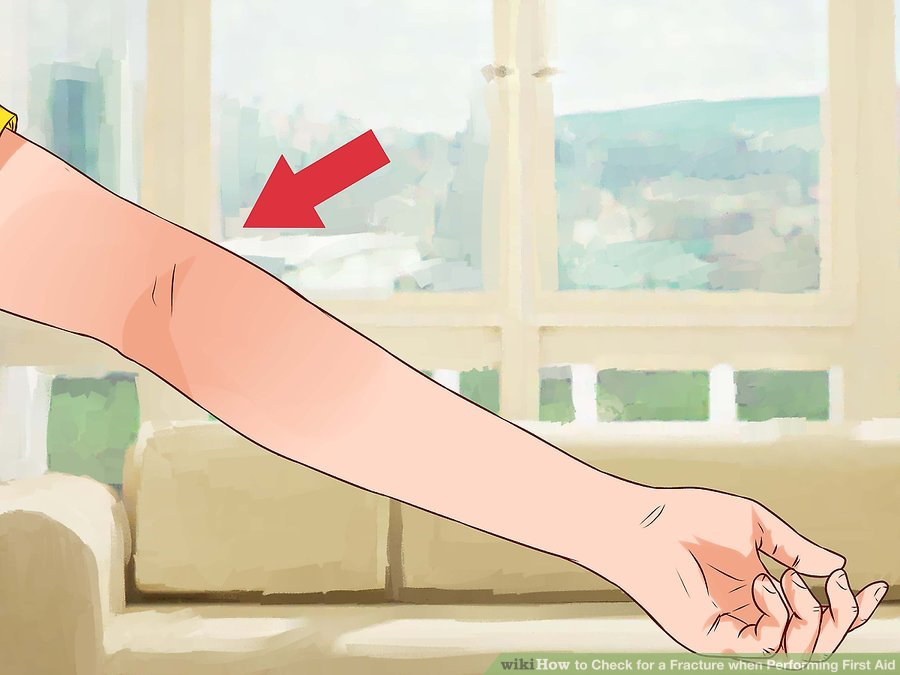
1. Check for a crooked limb
While some serious fractures poke through the skin (called an open fracture), most remain hidden underneath the skin (called closed fractures). Take a look at the injured person's limbs and neck and check for unnatural angles or positions that likely indicate a fracture or dislocation. Look for a limb that looks shorter, twisted or bent in an unnatural looking way.
- It's important not to move the neck, head or spine if it looks crooked or misaligned because you could cause permanent nerve damage and make the situation worse.
- While looking for deformities, compare side-to-side (left leg to right leg, for example) to better notice anything strange or unusual that’s indicative of a broken bone.
- Noticing an open fracture is much easier due to it poking out of the skin. Open fractures are considered more serious due to significant blood loss and risk of infection.
- You may have to loosen or remove some clothes to check thoroughly, but make sure to ask permission if the person is conscious.
2. Look for swelling and redness
A fractured bone is a major injury that requires lots of force, so expect to see swelling, redness and/or bruising. The inflammation and color changes develop quickly near the fracture site, so you shouldn’t have to wait very long to see them. Again, some clothing removal is likely necessary to see swelling.
- Swelling produces a visible lumpiness, inflating or ballooning of tissue around the broken bone, but don't mistake it for fat deposit. Swelling makes the skin tight and warm to the touch, whereas fat is jiggly and cool to the touch.
- Swelling and color changes happen due to broken blood vessels that bleed into surrounding areas beneath the skin. Red, purple and dark blue are common colors associated with broken bones.
- An open fracture causes external (visible) bleeding, which should be easy to see because it will soak through most types of fabrics pretty quickly.

3. Try to assess the pain
Although broken bones tend to be very painful (even small hairline / stress fractures), using pain to gauge an injury in an emergency situation can be tricky. First of all, the person may feel varying degrees of pain all over her body, depending on what happened to her. Secondly, the person may be unconscious or in shock and be unable to answer your questions or pinpoint any pain. So, certainly ask the injured person about her pain, but don't rely on it to check for a fracture.
- Gently touch (palpate) the person's limbs and torso (especially around the ribs) and look for any wincing if she is conscious but not communicating clearly.
- If the person is unconscious, then a pain assessment can't be done.
- Pain sensations can be greatly enhanced (from fear) or reduced (from adrenaline) when people are hurt, so it's not always reliable for an injury assessment.

4. Notice difficulty moving body parts
If the injured person is conscious and alert, ask him to carefully and slowly move arms, hands, feet and legs. If he has lots of difficulty and pain with movement, then a fracture or dislocation is possible. You may also hear a grating or cracking noise, which indicates the broken pieces of the bone are rubbing together.
- Ask him to start with wiggling his toes, then bending his knees, then lifting his legs off the ground, then moving his hands and arms.
- Even if the person can move his limbs (suggesting the spinal cord has not been injured), there may be damage to the bones of the spine. Unless it is necessary to get the person out of immediate danger, patients should not be moved until assessed by a medical professional due to the risk of paralyzing a patient.
- Loss of strength in a limb, even with some movement, is another indication of a fracture or dislocation, or a spine or nerve injury.

5. Ask about numbness and tingling
Typically when a bone is broken, especially the larger upper bones of the arms and legs, nerves are also injured or at least stretched and irritated. This produces electric-like pain, but also numbness or "pins and needles" below the site of the injury. Ask the injured person about the sensations in her hands and feet.
- Loss of sensation in the limbs indicate some type of nerve involvement, either in a peripheral nerve running down the leg / arm, or a spinal nerve within the spinal column.
- In addition to numbness and pins and needles, she may also feel strange temperature changes — either too cold or burning hot sensations.

Part 2: Addressing the Broken Bone
1. Don't move the fractured bone
If you think an injured person has a bone fracture (or dislocated joint), you should not move it in order to assess or treat it. Instead, you should continue with your basic first-aid treatment while the broken bone is in the position you found it or a more comfortable position chosen by the injured person. Without emergency medical training, moving a broken bone is just too risky.
- Discourage the injured person from moving around too much. Slightly changing position for comfort is fine, but trying to get up (especially if he is in shock) risks further injury.
- Supporting the injured body part for comfort or to stop the person from moving it is fine. Use a pillow, cushion or rolled up jacket or towel.

2. Stop any bleeding
There's not much you can do to stop the internal bleeding that invariably occurs with a closed fracture, but stopping or slowing down the bleeding from an open fracture is necessary and can be life saving. Apply pressure to the open wound with a sterile bandage, clean cloth or a clean piece of clothing until it stops bleeding and starts to clot — it can take up to five minutes or more, depending on the wound and which blood vessels are damaged.
- Protect yourself and the patient from blood-borne disease by wearing gloves. Coming into contact with the injured person's blood puts you at risk for disease like hepatitis, HIV, and other viral infections.
- Even if the fracture is closed, there may be surrounding cuts and abrasions that are bleeding and need attention.
- For an open fracture, once the bleeding is under control, cover the wound with a sterile dressing or something clean (to help prevent infection and debris getting in there) and secure it with a bandage. Do not remove the bandage or cloth you used to stop the bleeding — simply lay the new dressing over the old.
- You can lightly rinse the wound with water to remove any dirt or debris, but don't vigorously scrub it because it will make it bleed more.

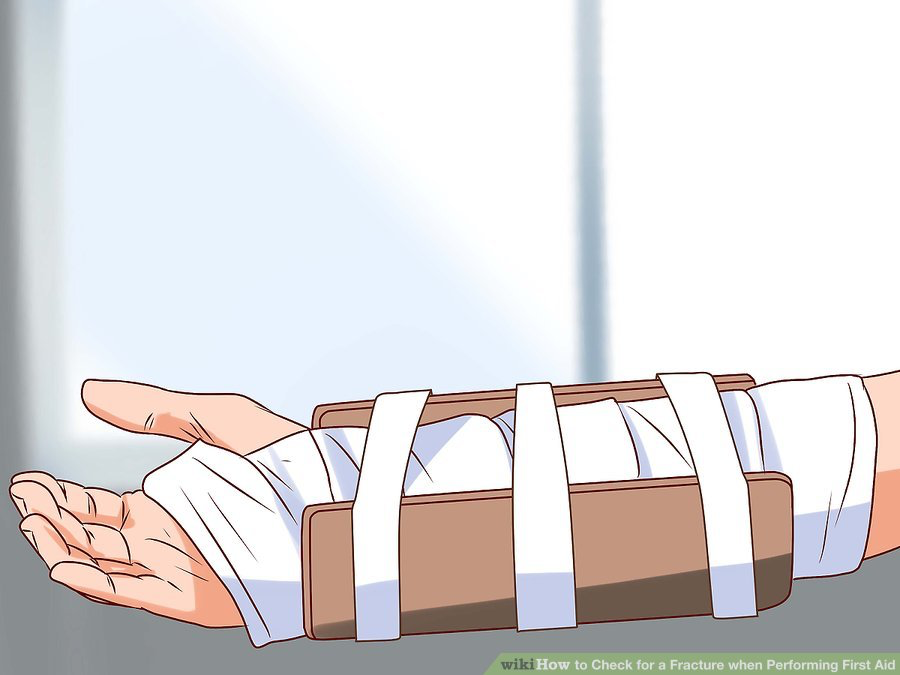
3. Immobilize the injured area
Never try to realign a broken bone or push it back into the body if it's sticking out. Instead, immobilize (secure) the broken bone with a splintor or sling, particularly if you've had any sort of emergency medical training. Potential material you can use for splints include rolled up newspapers or strips of wood. Remember to immobilize the area both above and below the fracture.
- Secure the splints around the arm or leg with elastic bandages (Ace or Tensor bandages), rope, a belt or strips of cloth or items of clothing. Don't tie it too tight and cut off circulation.
- Padding the splints with cloth or large bandages can help reduce discomfort.
- Consider making a simple sling to support a broken arm. Use a shirt and tie the sleeves around the person's neck for support.
- If you have no idea what a splint or sling are, then it's likely best not to try to make them. Stick with bleeding control and waiting for emergency services.
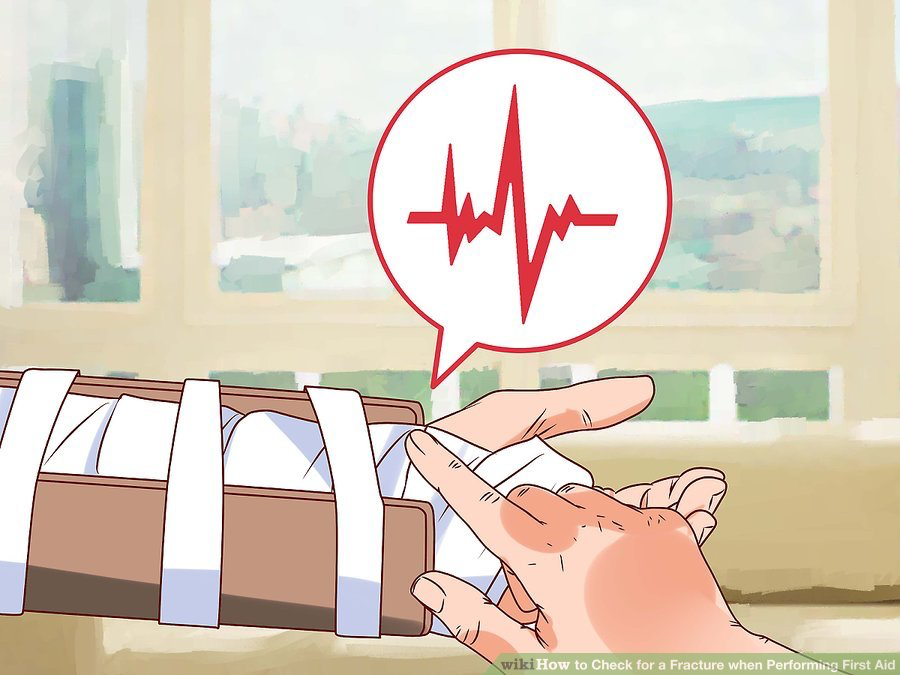
4. Monitor for circulation
If you decide to support a broken leg or arm with a splint and secure it with an Ace bandage or belt, you need to check for circulation every few minutes until help arrives. Tying the splint on too tight cuts off blood supply to the tissues downstream from the injury and can lead to tissue death from lack of oxygen and nutrients.
- Feel for a pulse in the wrist with a broken arm and the ankle area for a fractured leg. If you can't feel a pulse, loosen the ties on the splint and check again.
- You can also check visually. Press firmly over the skin downstream from the fracture site. It should first "blanch" white and then turn pink again in about two seconds.
- Signs of poor circulation include: pale or blueish skin, numbness or tingling and loss of pulse.
5. Apply cold therapy if possible
If you have any ice, frozen gel packs or bags of frozen veggies near by, apply them over the covered wound to help reduce (or limit) inflammation and numb the pain. Ice causes the small blood vessels to shrink a little so swelling is reduced. Ice will also help stop the bleeding of an open wound.
- Remember not to apply ice (or anything cold) directly to the skin. Always wrap the ice in a thin towel, piece of cloth or some other material before applying it to an injury.
- Leave the ice on for about 15 minutes or until emergency medical personnel arrive.

Part 3: Prioritizing First Aid Treatment
1. Call for help (see "EMERGENCY NUMBERS" above)
If you come across an emergency medical situation where people are injured, immediately call 10177 for an ambulance if nobody else has. Time is of the essence, so get help on the way first, then assess the injuries and deliver basic first aid while you're waiting for help to arrive. Precious lost minutes can make the difference between life and death, regardless of your level of first aid training.
- Even if people are seemingly not seriously injured, you should still call emergency services for help because you'll be unable to make an appropriate diagnosis due to either lack of training or necessary medical equipment.
- No one expects you to play doctor and fix any injuries. Focus on getting help to arrive and doing the basics — stopping any serious bleeding, offering support and trying to prevent shock (see below).

2. Survey the scene
Before you approach the injured person to administer first aid, you need to take a moment to look around and make sure there is no immediate danger. If you rush into a scene without checking for threats to your safety — like a downed electrical wire, falling debris, or a dangerous person — you may become injured yourself. Then all you have accomplished is giving emergency personnel two people to rescue instead of one.

3. Determine if the person is breathing
Once trained emergency medical help is called and on the way, assess whether an injured person is unconscious and/or not breathing. If the person is not breathing, giving her CPR is your top priority. Check the person's airway to see if it's blocked before giving CPR. Don't check for broken bones until the person is revived and breathing.
- If you do not have CPR training, you should not worry about administering rescue breaths — focus on chest compressions instead. If you are trained and confident in your abilities, then proceed with CPR that includes rescue breathing.
- Carefully position the person on her back and kneel next beside her, near her shoulders.
- Place the heel of your hand on the person's breastbone, between her nipples. Place your other hand on top of your first hand and use all your body weight to press down on the chest.
- Administer chest compressions at a rate of about 100 pumps per minute (imagine pressing to the rhythm of the Bee Gee's song "Stayin' Alive"). Give chest compressions until help arrives. If you become tired, see if someone can switch off with you.
- If you are trained in CPR, then check the person's airway after 30 compressions and begin to deliver rescue breathing.

4. Watch for shock
Once help is on the way, the person is breathing, bleeding is under control and you've stabilized any broken bones, you need to remain vigilant for shock. Shock is a physiological response to loss of blood, injury and pain, which can quickly become fatal if not properly addressed. Signs to look out for include: feeling faint, rapid shallow breathing, low blood pressure, confusion, strange / inappropriate behavior, loss of consciousness.
- To combat shock: control bleeding first, lay the person down with his head slightly lower than his torso, elevate his legs, keep him warm with a blanket and offer him liquids to drink if he is able.
- Calm him down by not panicking yourself and make sure he knows that help is on the way.
- Reassure him that he'll be okay (even if you don't think he will be) and distract him from looking at his injuries.

_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
