Back Conditions Explained
Jaundice

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Roger Henderson (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
When you are jaundiced it means that your skin and other body parts turn a yellow colour. It is due to a build-up of a chemical called bilirubin in the tissues of the body. There are many conditions that can cause jaundice - some more serious than others. Always see a doctor if you become jaundiced, as it is vital to diagnose the cause. The treatment and outlook (prognosis) depend on the cause.
What is jaundice?
When you are jaundiced it means that your skin and other body parts turn a yellow colour. It is due to a build-up of a chemical called bilirubin in the tissues of the body. Bilirubin is a normal body chemical but can build up to abnormally high levels in various diseases. The whites of the eyes are often the first tissues that you notice turning yellow when you develop jaundice. If the bilirubin level is only mildly high then this might be the only part of the body where you can detect a yellow colour. With higher levels of bilirubin, the skin also becomes yellow.

Understanding bilirubin - the cause of the yellow colour
You have millions of red blood cells in your bloodstream. Each blood cell lasts for about 120 days and is then broken down by cells in the body into various waste chemicals. (New red blood cells are being made all the time to replace the ones being broken down.) Bilirubin is one of the chemicals that comes from the broken down red cells.
Bilirubin is carried around the bloodstream. As the blood flows through the liver, the liver cells take up the bilirubin. Chemicals in the liver cells slightly alter the structure of the bilirubin to make it water-soluble. This water-soluble bilirubin is called conjugated bilirubin. (The bilirubin in the blood before being taken up by liver cells is called unconjugated bilirubin).
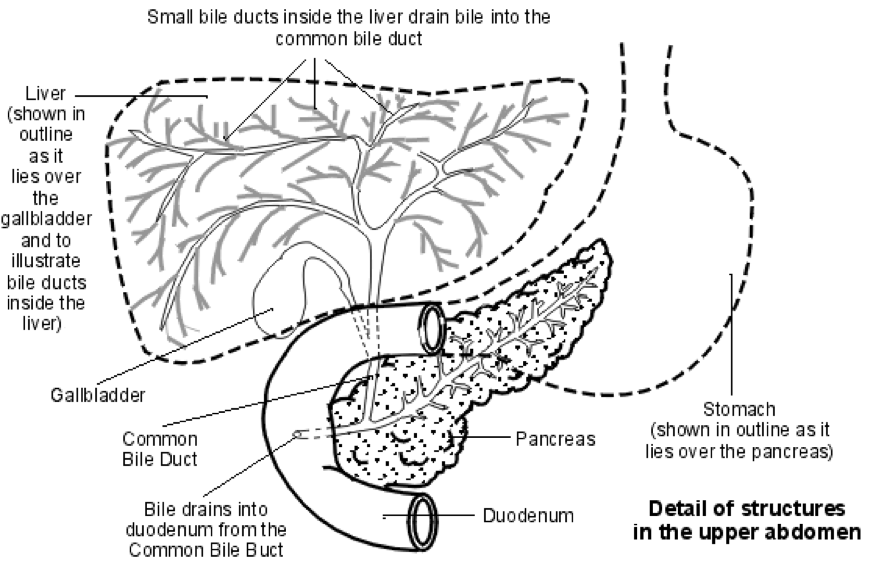
The liver cells pass out the conjugated bilirubin into tiny tubes called bile ducts. The bilirubin is therefore now part of bile. Bile is a mix of various waste chemicals passed out by the liver cells. (One function of liver cells is to get rid of a range of waste chemicals in the bile).
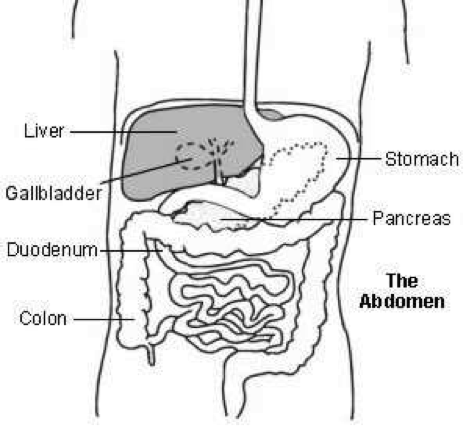
There is a network of bile ducts in the liver. They join together (like branches of a tree) to form the larger common bile duct. Bile constantly drips down the tiny bile ducts, into the common bile duct and into the first part of the gut (small intestine), known as the duodenum).
The gallbladder lies under the liver. It is like a pouch off the common bile duct, which stores bile. The gallbladder squeezes (contracts) when we eat. This empties the stored bile back into the common bile duct and out into the duodenum. The bilirubin in the bile gives the poo (faeces) the typical brown colour.
So, getting rid of bilirubin is a normal process. It is when abnormal amounts of bilirubin build up in the blood that you become jaundiced. And this can happen for many different reasons.
Jaundice causes
It is useful to divide the causes of jaundice into four general areas:
- Conditions affecting the red blood cells.
- Conditions affecting the liver cells.
- Conditions affecting the tiny bile ducts within the liver.
- Conditions affecting the common bile duct outside the liver.
Conditions affecting the red blood cells
Various conditions cause an increased rate of breakdown of red blood cells. As a result, there is more bilirubin made than usual which then circulates in the blood. The liver cells are unable to keep pace and process the extra bilirubin. Therefore, a backlog of bilirubin builds up in the blood awaiting the liver cells to process it. This increased amount of bilirubin then spills into the tissues of the body to cause jaundice.
Conditions that cause an increased rate of breakdown of red blood cells include:
- Some genetic diseases such as sickle cell anaemia, thalassemia, spherocytosis, and glucose 6-phosphate dehydrogenase deficiency. Genetic means that the condition is passed on through families through special codes inside cells called genes.
- Haemolytic uraemic syndrome.
- Malaria.
Conditions affecting the liver cells
There are many conditions that affect the liver cells. In some conditions the liver cells are unable to take in the bilirubin very well, so bilirubin builds up in the bloodstream. Sometimes there is a problem with the chemicals (enzymes) within the liver cells that process the bilirubin. Sometimes there is a problem in the way the liver cells pass out the processed bilirubin into the bile ducts. Sometimes, the liver cells are just damaged and all processes of the cell do not work well, or there are a reduced number of liver cells that are working. With these problems, bilirubin may spill into the bloodstream to cause jaundice.
Conditions affecting liver cells that may cause jaundice include:
- Hepatitis: This means inflammation of the liver. There are many causes such as:
- Infection with one of the hepatitis viruses.
- Some infections with germs (bacterial infections).
- Alcoholic hepatitis.
- Autoimmune hepatitis.
- Inflammation caused by poisons or as a side-effect of some medicines.
- Cirrhosis: This is a condition where normal liver tissue is replaced by scar tissue (fibrosis). It tends to progress slowly and often does not cause symptoms in its early stages. However, as the function of the liver gradually becomes worse, serious problems can develop and jaundice may occur.
- Inherited (hereditary) defects in the enzymes that process bilirubin in liver cells. These include Gilbert's syndrome, Dubin-Johnson syndrome, Crigler-Najjar syndrome and Rotor's syndrome. Gilbert's syndrome is very common, affecting about 1 in 20 people. It typically causes only very mild jaundice from time to time. The other hereditary defects are rare.
Conditions affecting the tiny bile ducts
If the tiny bile ducts within the liver become damaged or narrowed then the flow of bile is restricted. A backlog of bile (which contains bilirubin) then spills into the bloodstream. Various conditions can affect or damage the bile ducts in this way. For example, primary biliary cirrhosis, primary sclerosing cholangitis and as a side-effect of some medicines.
Conditions affecting the common bile duct
The bile from all the tiny bile ducts in the liver drains into the common bile duct. If the common bile duct becomes narrowed or blocked (obstructed) then bile which contains bilirubin can seep out into the bloodstream and cause jaundice. This is sometimes called obstructive jaundice or post-hepatic jaundice (hepatic is another word for liver).
Conditions that can cause this include:
- Gallstones: These occur when bile, which is normally fluid, forms stones. Most gallstones form in the gallbladder and do not cause any problem. Jaundice is an uncommon complication of gallstones. It occurs if a gallstone comes out of the gallbladder but gets stuck in the common bile duct. Bile then cannot pass into the gut and so seeps into the bloodstream.
- Pancreatic cancer in the head of the pancreas, which can block the flow of bile.
- Inflammation of the pancreas (pancreatitis): This can cause swelling of the pancreas, which may block the flow of bile. See separate leaflets called Acute Pancreatitis and Chronic Pancreatitis for more details.
- Biliary atresia: In this condition, part or all of the bile ducts become inflamed. This then leads to scarring (fibrosis) and narrowing and blockage of the bile ducts. The cause is not clear.
- Cancer of the gallbladder: This may grow to block the common bile duct.
Diagnosis
What assessment and tests may be done?
If you become jaundiced you should see your doctor. As discussed above, there are various causes. Some are more common than others and some are more serious than others. It is vital to obtain the correct diagnosis, as the treatment and outlook (prognosis) can vary greatly, depending on the cause. However, sometimes, finding the cause can be a bit of a detective process and is not always easy or straightforward.
Your doctor is likely to ask various questions if you become jaundiced. He or she will also examine you. On the basis of this assessment, the possible causes may become clear, as certain symptoms and signs are associated with some causes of jaundice and not with others.
However, tests are usually needed to confirm an exact diagnosis:
- Various blood tests are usually done. These will show whether the raised level of bilirubin is unconjugated or conjugated (as discussed earlier). This can help to narrow down the possible causes of jaundice. Blood tests, called liver function tests, can also measure various liver enzymes which help to show if the liver is inflamed or working well. Blood tests can also detect certain viruses or markers of other infections that can affect the liver. Various other more detailed blood tests may be needed.
- Urine tests may help to show if the the levels of various chemicals in the blood are raised. This can help to narrow down the possible causes of jaundice.
- An ultrasound scan of the liver, common bile duct and pancreas may identify a cause. In particular, it can often identify the cause of any blockage to the common bile duct. For example, a gallstone or cancer of the pancreas.
- An MRI scan of the liver may be useful.
- Taking a sample of the liver (a liver biopsy). This is taken to look at under the microscope.
- Other more complex tests may be needed if the diagnosis is still in doubt.
Jaundice in newborn babies
Always get a doctor to see a baby who is jaundiced. It is often not serious but some cases are serious and need further tests and treatment. Jaundice in newborn babies can be divided up into common simple (physiological) jaundice and other causes.
Physiological jaundice:
It is common for newborn babies to develop mild jaundice when they are 2-3 days old. It is due to a mild increase in the breakdown of red blood cells combined with a liver that is not quite fully functioning. The liver soon matures and the jaundice begins to disappear towards the end of the first week and has gone by day 10. The baby is well and has no other problems.
Other causes:
The are various other causes of jaundice in newborn babies. Some are due to serious disease of the blood or liver or to other problems. As a rule, the jaundice is not likely to be physiological jaundice if the baby is unwell and/or the jaundice is present in the first 24 hours after birth or lasts for more than 10 days.
Jaundice treatment
The treatment depends on the cause.
About the author
Dr Roger Henderson
GP
Dr Roger Henderson qualified as a doctor and a general practitioner from St Bartholomew's Hospital, London. He appears regularly on television and radio and has written multiple books. His full-time medical responsibilities include being a senior partner of a six doctor general practice in Shropshire, running a main surgery and two branch surgeries, as well as teaching medical students and GP registrars.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
