Back Conditions Explained
Slipped Disc
Also known as Sciatica or Prolapsed Disc
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Colin Tidy (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
A 'slipped' (prolapsed) disc often causes severe lower back pain. The disc often presses on a nerve root which can cause pain and other symptoms in a leg. In most cases, the symptoms ease off gradually over several weeks. The usual advice is to do normal activities as much as possible. Painkillers may help. Physical treatments such as spinal manipulation may also help. Surgery may be an option if the symptoms persist.
Understanding the back
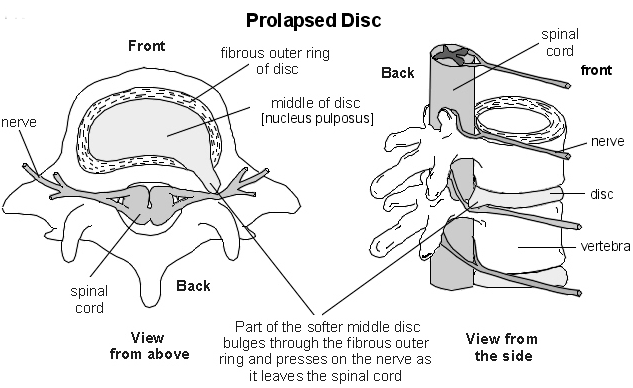
The spine is made up of many bones called vertebrae. These are roughly circular and between each vertebra is a disc. The discs are made of strong rubber-like tissue which allows the spine to be fairly flexible. A disc has a stronger fibrous outer part and a softer jelly-like middle part called the nucleus pulposus.
The spinal cord, which contains the nerves that come from the brain, is protected by the spine. Nerves from the spinal cord come out from between the vertebrae to relay messages to and from various parts of the body.
Strong ligaments attach to the vertebrae. These give extra support and strength to the spine. Various muscles also surround, and are attached to, various parts of the spine. (The muscles and ligaments are not shown in the diagram below, for clarity.)
What is a prolapsed disc?
When you have a 'slipped' (prolapsed) disc, a disc does not actually ‘slip’. What happens is that part of the inner softer part of the disc (the nucleus pulposus) bulges out (herniates) through a weakness in the outer part of the disc. A prolapsed disc is sometimes called a herniated disc. The bulging disc may press on nearby structures such as a nerve coming from the spinal cord. Some inflammation also develops around the prolapsed part of the disc.
Any disc in the spine can prolapse. However, most prolapsed discs occur in the lower back (the lumbar spine). The size of the prolapse can vary. As a rule, the larger the prolapse, the more severe the symptoms are likely to be.
Who gets a prolapsed disc?
Bouts of back pain are very common. However, less than 1 in 20 cases of sudden-onset (acute) back pain are due to a 'slipped' (prolapsed) disc. (Most cases of back pain are classed as simple low back pain. This is thought to be caused by a minor problem in a muscle, ligament, or other structure in the back - for example, a strained muscle.
The most common age to develop a prolapsed disc is between 30 and 50 years. Twice as many men as women are affected.
Causes
What causes a prolapsed disc?
It is not clear why some people develop a 'slipped' (prolapsed) disc and not others, even when they do the same job or lift the same sort of objects. It seems that some people may have a weakness in the outer part of the affected disc. Various things may trigger the inner softer part of the disc to prolapse out through the weakened outer part of the disc. For example, sneezing, awkward bending, or heavy lifting in an awkward position may cause some extra pressure on the disc. In people with a weakness in a disc, this may be sufficient to cause a prolapse.
Factors that may increase the risk of developing a prolapsed disc include:
- A job involving lots of lifting.
- A job involving lots of sitting (especially driving).
- Weight-bearing sports (weightlifting, etc).
- Smoking.
- Being overweight (obesity).
- Increasing age (a disc is more likely to develop a weakness with increasing age).
Symptoms
What are the symptoms of a prolapsed disc?
Back pain
The pain is often severe and usually comes on suddenly. The pain is usually eased by lying down flat and is often made worse if you move your back, cough or sneeze.
Nerve root pain (usually sciatica)
Nerve root pain is pain that occurs because a nerve coming from the spinal cord is pressed on (trapped) by a 'slipped' (prolapsed) disc, or is irritated by the inflammation caused by the prolapsed disc. Although the problem is in the back, you feel pain along the course of the nerve in addition to back pain. Therefore, you may feel pain down a leg to the calf or foot. Nerve root pain can range from mild to severe, but it is often worse than the back pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. (The term sciatica means nerve root pain of the sciatic nerve.) The sciatic nerve is a large nerve that is made up from several smaller nerves that come out from the spinal cord in the lower back. It travels deep inside the buttock and down the back of the leg. There is a sciatic nerve for each leg.
Other nerve root symptoms
The irritation or pressure on the nerve next to the spine may also cause pins and needles, numbness or weakness in part of a buttock, leg or foot. The exact site and type of symptoms depend on which nerve is affected.
Cauda equina syndrome - rare, but an emergency
Cauda equina syndrome is a particularly serious type of nerve root problem that can be caused by a prolapsed disc. This is a rare disorder where the nerves at the very bottom of the spinal cord are pressed on.
This syndrome can cause low back pain plus:
- Problems with bowel and bladder function (usually inability to pass urine).
- Numbness in the saddle area around the back passage (anus).
- Weakness in one or both legs.
This syndrome needs urgent treatment to preserve the nerves to the bladder and bowel from becoming permanently damaged. See a doctor immediately if you develop these symptoms.
The absence of symptoms
Research studies where routine back scans have been done on a large number of people have shown that some people have a prolapsed disc without any symptoms. It is thought that symptoms mainly occur if the prolapse causes pressure on or irritation of a nerve. This does not happen in all cases. Some prolapses may be small or occur away from the nerves and cause minor or no symptoms.
Progression
How does a prolapsed disc progress?
In most cases, the symptoms tend to improve over a few weeks. Research studies of repeated MRI scans have shown that the bulging prolapsed portion of the disc tends to get smaller (regress) over time in most cases. The symptoms then tend to ease and, in many cases, go. In only about 1 in 10 cases is the pain still bad enough after six weeks to consider surgery (see below).
Diagnosis
Do I need any tests?
Your doctor will normally be able to diagnose a 'slipped' (prolapsed) disc from the symptoms and by examining you. (It is the common cause of sudden back pain with nerve root symptoms.) In most cases, no tests are needed, as the symptoms often settle within a few weeks.
Tests such as X-rays or scans may be advised if symptoms persist. In particular, an MRI scan can show the site and size of a prolapsed disc. This information is needed if treatment with surgery is being considered.
Treatment
What are the treatments for a prolapsed disc?
Exercise and keep going
Continue with normal activities as far as possible. This may not be possible at first if the pain is very bad. However, move around as soon as possible and get back into normal activities as soon as you are able. As a rule, don't do anything that causes a lot of pain. However, you will have to accept some discomfort when you are trying to keep active. Setting a new goal each day may be a good idea - for example, walking around the house on one day, a walk to the shops the next, etc.
In the past, advice had been to rest until the pain eases. It is now known that this was wrong. You are likely to recover more quickly and are less likely to develop persistent (chronic) back pain if you keep active when you have back pain rather than rest a lot. Also, sleep in the most naturally comfortable position on whatever is the most comfortable surface. (Advice given in the past used to be to sleep on a firm mattress. However, there is no evidence to say that a firm mattress is better than any other type of mattress for people with back pain).
Medication
If you need painkillers, it is best to take them regularly. This is better than taking them now and again just when the pain is very bad. If you take them regularly the pain is more likely to be eased for much of the time, enabling you to exercise and keep active.
- Paracetamol is often sufficient if you take it regularly at full strength.
- Anti-inflammatory painkillers: Some people find that these work better than paracetamol. They include ibuprofen which you can buy at pharmacies or obtain on prescription. Other types such as diclofenac or naproxen need a prescription. Some people with asthma, high blood pressure, kidney failure, or heart failure may not be able to take anti-inflammatories.
- A stronger painkiller such as codeine is an option if anti-inflammatories do not suit or do not work well. Codeine is often taken in addition to paracetamol. Constipation is a common side-effect from codeine. This may make back pain worse if you need to strain to go to the toilet. To prevent constipation, have lots to drink and eat foods with plenty of fibre.
- A muscle relaxant is sometimes prescribed for a few days if the back muscles become very tense and make the pain worse.
Physical treatments
Some people visit a physiotherapist, chiropractor or osteopath for manipulation and/or other physical treatments. It is debatable whether physical treatments would help all people with a 'slipped' (prolapsed) disc. However, physical treatments provide some short-term comfort and hasten recovery in some cases.
Surgery
Surgery may be an option in some cases. As a rule, surgery may be considered if the symptoms have not settled after about six weeks or so. This is the minority of cases as, in about 9 in 10 cases, the symptoms have eased off and are not bad enough to warrant surgery within about six weeks.
The aim of surgery is to remove the prolapsed part of the disc. This often eases symptoms. However, it does not work in every case. Also, as with all operations, there is a risk from surgery. A specialist will advise on the pros and cons of surgery and on the different techniques that are available.
Prevention
Can further bouts of back pain and/or prolapsed disc be prevented?
Evidence suggests that the best way to prevent bouts of back pain and 'slipped' (prolapsed) disc is simply to keep active and to exercise regularly. This means general fitness exercise such as walking, running, swimming, etc. There is no firm evidence to suggest that any particular back strengthening exercises are more useful than simply keeping fit and active. It is also sensible to be back-aware. For example, do not lift objects when you are in an awkward twisting posture.
About the author
Dr Colin Tidy
MBBS, MRCGP, MRCP, DCH
Dr Colin Tidy qualified as a doctor in 1983 and he has been writing for Patient since 2004. Dr Tidy has 25 years’ experience as a General Practitioner. He now works as a GP in Oxfordshire, with a special interest in teaching doctors and nurses, as well as medical students. In addition to writing many leaflets and articles for Patient, Dr Tidy has also contributed to medical journals and written a number of educational articles for General Practitioner magazines.
Recommended websites
For further reading go to:
- Investigating the spine - the role of a MRI Scan
- Spinal Stenosis – narrowing of the spinal canal
- More about the Cauda Equina Syndrome
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
