Back Conditions Explained
Ovarian Cyst

We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient Uk, authored by Dr Mary Harding (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
Overview
The vast majority of ovarian cysts are non-cancerous (benign), but some are cancerous (malignant) or may become cancerous over time.
What are the ovaries?
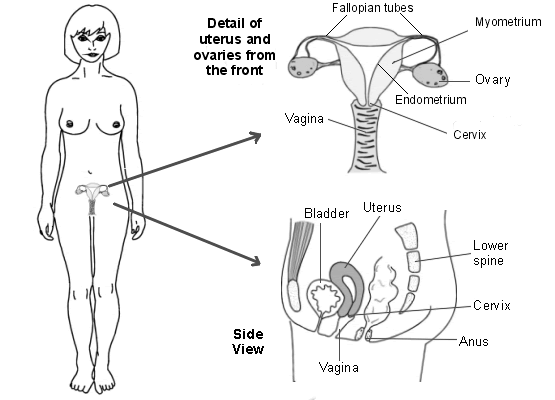
Women have two ovaries, one on either side of the womb (uterus) in the lower tummy (abdomen). Ovaries are small and round, each about the size of a walnut. The ovaries make eggs. In fertile women, each month an egg (ovum) is released from one of the ovaries. The egg passes down the Fallopian tube into the uterus where it may be fertilised by a sperm.
The ovaries also make chemicals (hormones) including the main female hormones - oestrogen and progesterone. These hormones pass into the bloodstream and have various effects on other parts of the body, including regulating the menstrual cycle and periods.
Ovulation
In women of childbearing age, an egg forms and matures each month in a tiny structure within an ovary, called a follicle. When the egg is released (at ovulation) the follicle turns into a small structure called a corpus luteum. If you become pregnant, the corpus luteum forms hormones to help with the pregnancy. If you do not become pregnant, the corpus luteum shrinks and goes away within a couple of weeks.
What are ovarian cysts?
A cyst is a fluid-filled sac. Cysts develop in various places in the body. Depending on the type of cyst, the fluid within the cyst can range from thin and watery to thick and paste-like. Some cysts have a thicker solid outer part with some fluid within.
Cysts on the ovary are very common. Ovarian cysts can vary in size - from less than the size of a pea to the size of a large melon (occasionally even larger).
There are various types which include the following:
Functional ovarian cysts
These are the most common type. They form in some women of childbearing age (women who still have periods) when there is a functional fault with ovulation. They are very common.
There are two types:
- Follicular cysts: A follicle (see "Ovulation", above) can sometimes enlarge and fill with fluid. They can occur commonly in women who are receiving infertility treatment.
- Corpus luteum cysts: These occur when the corpus luteum (see "Ovulation", above) fills with fluid or blood to form a cyst. A blood-filled cyst is sometimes called a haemorrhagic cyst.
Both of these cysts can grow up to about 6 cm across. They usually do not need treatment, as they normally go away on their own within a few months.
Other cysts less common:
Dermoid cysts
(sometimes called benign mature cystic teratomas)
Dermoid cysts tend to occur in younger women. These cysts can grow quite large - up to 15 cm across. These cysts often contain odd contents such as hair, parts of teeth or bone, fatty tissue, etc. This is because these cysts develop from cells which make eggs in the ovary. An egg has the potential to develop into any type of cell. So, these cysts can make different types of tissue. In about 1 in 10 cases a dermoid cyst develops in both ovaries. Dermoid cysts can run in families.
Cystadenomas
These develop from cells which cover the outer part of the ovary. There are different types. For example, serous cystadenomas fill with a thin fluid and mucinous cystadenomas fill with a thick mucous-type fluid. These types of cysts are often attached to an ovary by a stalk rather than growing within the ovary itself. Some grow very large. They are usually benign, but some are cancerous.
Endometriomas
Many women who have endometriosis develop one or more cysts on their ovaries. Endometriosis is a condition where endometrial tissue (the tissue that lines the womb (uterus)) is found outside the uterus. It sometimes forms cysts which fill with blood. The old blood within these cysts looks like chocolate and so these cysts are sometimes called chocolate cysts. They are benign.
Polycystic ovary syndrome (PCOS)
Polycystic means many cysts. If you have PCOS you develop many tiny benign cysts in your ovaries. The cysts develop due to a problem with ovulation, caused by a hormonal imbalance. PCOS is associated with period problems, reduced fertility, hair growth, obesity, and acne.
Others
There are also other rare types of ovarian cysts. There are also various types of benign ovarian tumours which are solid and not cystic (do not have fluid in the middle).
Symptoms, Problems & Complications
What are the symptoms, problems and possible complications?
Most ovarian cysts are small, non-cancerous (benign), and cause no symptoms.
Some ovarian cysts cause problems which may include one or more of the following:
- Pain or discomfort in the lower tummy (abdomen). The pain may be constant or intermittent. Pain may only occur when you have sex.
- Periods sometimes become irregular or may become heavier or lighter than usual.
- Sometimes a cyst may bleed into itself or burst. This can cause a sudden severe pain in the lower abdomen.
- Occasionally, a cyst which is growing on a stalk from an ovary may twist the stalk on itself (a torsion). This stops the blood flowing through the stalk to the cyst and causes the cyst to lose its blood supply. This can cause sudden severe pain in your lower abdomen.
- Large cysts can cause your abdomen to swell or press on nearby structures. For example, they may press on your bladder or rectum, which may cause urinary symptoms or constipation.
- Although most cysts are benign, some types have a risk of becoming cancerous.
- Rarely, some ovarian cysts make abnormal amounts of female (or male) chemicals (hormones) which can cause unusual symptoms.
Diagnosis
How is an ovarian cyst diagnosed?
As most ovarian cysts cause no symptoms, many cysts are diagnosed by chance - for example, during a routine examination, or if you have an ultrasound scan for another reason.
If you have symptoms suggestive of an ovarian cyst, your doctor may examine your tummy (abdomen) and perform an internal (vaginal) examination. He or she may be able to feel an abnormal swelling which may be a cyst.
An ultrasound scan can confirm an ovarian cyst. An ultrasound scan is a safe and painless test which uses sound waves to create images of organs and structures inside your body. The probe of the scanner may be placed on your abdomen to scan the ovaries. A small probe is also often placed inside your vagina to scan your ovaries, to obtain more detailed images.
Your doctor may also take samples of your blood and urine. Some women may have other tests - for example, a CT or MRI scan.
Treatment
What is the treatment for ovarian cysts?
Your GP will advise on the best course of action or refer you to a specialist. This depends on factors such as:
- Your age.
- Whether you are past the menopause.
- The appearance and size of your cyst from the ultrasound scan.
- Whether you have any symptoms.
Observation
Many small ovarian cysts will resolve and disappear over a few months, which means your doctor with tell you to do or take nothing. You may be advised to have a repeat ultrasound scan after a few months or so. If the cyst goes away, then no further action is needed.
Operation
Removal of an ovarian cyst may be advised, especially if you have symptoms or if the cyst is large. Sometimes the specialist may want to remove it to determine exactly which type of cyst it is and to make sure there are no cancer cells in it. Most smaller cysts can be removed by 'keyhole' (laparoscopic) surgery. Some cysts require a more traditional style of operation.
The type of operation depends on factors such as the type of cyst, your age, and whether cancer is suspected or ruled out. In some cases, just the cyst is removed, and the ovary tissue preserved. In some cases, the ovary is also removed, and sometimes other nearby structures such as the womb (uterus) and the other ovary. Your specialist will advise on the options for your individual situation.
About the author
Dr Mary Harding
BA, MA, MB BChir, MRCGP, DFFP
Mary qualified at Cambridge in 1989. She joined EMIS as an author in 2013. Mary is a part-time, salaried GP at The Village Surgery, Wheathampstead and previously for 12 years in Welwyn Garden City. Mary is also an appraiser and Senior Appraiser for NHS England, in the Central Midlands area team.
Recommended websites
For further reading go to:
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
