Back Procedures Explained
Disclaimer:
This website is intended to assist with patient education and should not be used as a diagnostic, treatment or prescription platform or service. Always refer any concerns or questions about diagnosis, treatment or prescription to your doctor.
Bronchoscopy
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website Patient UK, authored by Dr Oliver Starr, reviewed by Prof Cathy Jackson (see below). Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is a bronchoscopy?
A bronchoscopy is a test where a doctor looks into your lungs with a thin, plastic camera tube.
Bronchoscope:

Image by Håkon Olav Leira (Own work) via Wikimedia Commons
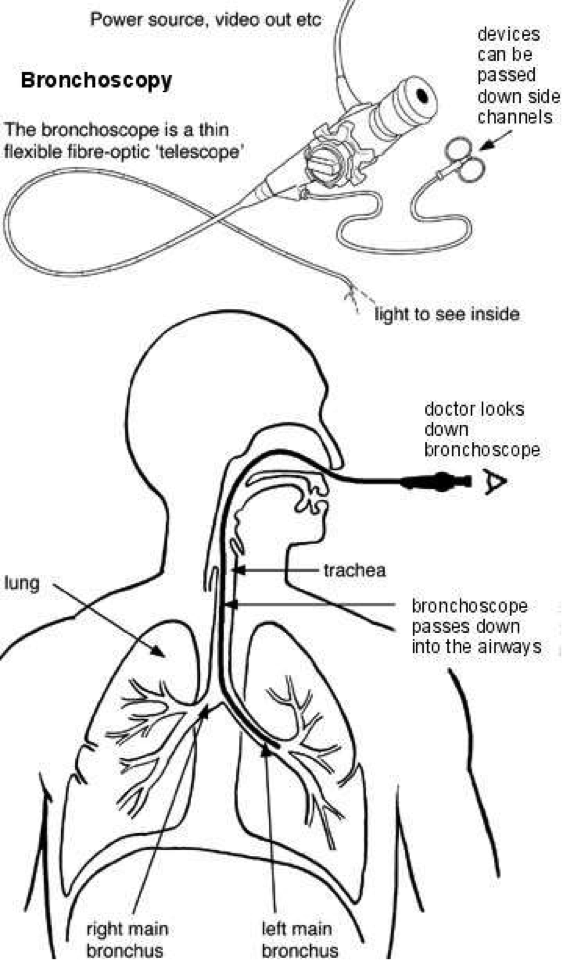
A fibre-optic bronchoscope is the device usually used. This is a thin, flexible, telescope (shown in the diagram). It is about as thin as a pencil. You are usually awake during a bronchoscopy, but usually are sedated and made very sleepy. It is not painful.
The bronchoscope is passed through your nose or mouth, down the back of your throat, into your windpipe (trachea), and down into your bronchi. The fibre-optics allow light to shine around bends in the bronchoscope and so the doctor can see clearly inside your airways.
A rigid bronchoscope (not shown in diagram) is used much less often. It is like a thin, straight telescope. It may be needed for some procedures and in children. It requires a general anaesthetic. (A fibre-optic bronchoscopy only requires sedation).
Both types of bronchoscope have a side channel down which thin instruments can pass. For example, a thin grabbing instrument can pass down to take a small sample (biopsy) from the inside lining of an airway, or from structures next to the airways.
Who has a bronchoscopy?
To help diagnose a problem
There are various reasons for having a bronchoscopy. For example, to help make a diagnosis if you have a persistent cough or cough up blood and the cause is not clear. If you have a shadow on a chest X-ray or the doctor sees a growth or a strange-looking area in a bronchus, the doctor may take a small sample (a biopsy) during a bronchoscopy. The sample is then looked at under the microscope to help decide whether problems such as inflammation, infection or cancer might be responsible for your symptoms. Bronchial lavage (described below) is also sometimes done during a bronchoscopy to help diagnose certain lung conditions.
To treat various problems
As mentioned, thin instruments can be passed down the side channel of a bronchoscope. Different instruments can do different things - for example:
- To remove a small object (such as an inhaled peanut) that has been lodged in an airway.
- To insert a small tube called a stent to open a blocked airway.
- To remove a growth that is blocking an airway.
- To take a small biopsy of a growth to see what it is.
What happens during a bronchoscopy?
Bronchoscopy using a flexible bronchoscope
This is usually done as an outpatient or day case. The doctor will numb the inside of your nose and the back of your throat by spraying on some local anaesthetic. This may taste a bit unpleasant. Also, you will normally be given a sedative to help you to relax. This is usually given by an injection into a vein in the back of your hand or your arm. The sedative can make you drowsy, but it is not a general anaesthetic and does not make you go to sleep. However, you are unlikely to remember anything about the bronchoscopy if you have a sedative.
You may be connected to a monitor to check your heart rate and blood pressure during the procedure. A device called a pulse oximeter may also be put on a finger. This does not hurt. It checks the oxygen content of the blood and will indicate if you need extra oxygen during the bronchoscopy. You may have soft plastic tubes placed just inside your nostrils to give you oxygen during the procedure.
The doctor will insert the tip of the bronchoscope into one of your nostrils and then gently guide it round the back of your throat into your windpipe (trachea). (It is sometimes passed via your mouth rather than via your nose if you have narrow nasal passages). The bronchoscope may make you cough.
The doctor looks down the bronchoscope and inspects the lining of your trachea and main bronchi (the main airways). Bronchoscopes transmit pictures through a camera attachment on to a TV monitor for the doctor to look at.
The doctor may take one or more samples (biopsies) of parts of the inside lining of the airways - depending on why the test is done and what they see. This is painless. The biopsy samples are sent to the laboratory for testing and to be looked at under the microscope.
Sometimes bronchial lavage is done. This is a procedure where some fluid is squirted into a section of the lung and then syringed back. The fluid is then examined in the laboratory to look for abnormal cells and other particles that may be present in certain diseases.
The bronchoscope is then gently pulled out. Sometimes other procedures are done, as described earlier.
The bronchoscopy itself usually takes about 20-30 minutes. However, you should allow at least two hours for the whole appointment, to prepare, give time for the sedative to work, for the bronchoscopy itself and to recover.
Bronchoscopy using a rigid bronchoscopy
This requires a general anaesthetic, similar to that for minor operations. So, after receiving the anaesthetic, the next thing you know is when you wake up in a recovery room.
What preparation do I need to do?
You may be advised not to take any medicines that affect blood clotting, such as aspirin and warfarin, for one week before the bronchoscopy. (You will need to discuss your medication with your doctor if you take such medicines for other conditions).
In addition to this, you should receive instructions from the hospital before the test. These usually include:
- That you should not eat or drink for several hours before the bronchoscopy. (Small sips of water may be allowed up to two hours before the test.)
- That you will need somebody to accompany you home, as you will be drowsy with the sedative.
What can I expect after a flexible bronchoscopy?
If you have a sedative, you may take an hour or so before you are ready to go home after the bronchoscopy is finished. The sedative will normally make you feel quite pleasant and relaxed. However, you should not drive, operate machinery or drink alcohol for 24 hours after having the sedative. You should not eat or drink anything for two hours after the bronchoscopy because your throat will still be numb. You will need somebody to accompany you home and to stay with you for 24 hours until the effects have fully worn off. Most people feel able to resume normal activities after 24 hours.
The doctor may tell you what they saw before you leave. However, if you have had a sedative you may not remember afterwards what they said. Therefore, you may wish to have a relative or close friend with you who may be able to remember what was said. The result from any sample (biopsy) may take a few days or weeks to come back.
Are there any side-effects or possible complications?
Most are done without any problem. Your nose and throat may be a little sore for a day or so afterwards. You may feel tired or sleepy for several hours, caused by the sedative. There is a slightly increased risk of developing a throat or chest infection following a bronchoscopy.
If you had a biopsy taken, you may cough up a little blood a few times in the following day or so. Rarely, a bronchoscopy can cause damage to the lung. This is more likely to occur if a specialised sample (biopsy) of lung tissue is taken. Serious complications from a bronchoscopy are extremely rare.
About the author
Dr Oliver Starr
MBChB, BMedSc, MRCS, MRCGP, DRCOG
Dr Oliver Starr is a general practitioner in Hertfordshire. He is an undergraduate tutor at University College Medical School, a general practice appraiser and a case assessor at the National Perinatal Epidemiology Unit, University of Oxford. Other interests include medical law, particularly regarding clinical negligence. Dr Starr is a council member of the Cameron Fund charity.
Recommended websites
For further information go to:
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
