Back Conditions Explained
Cervical Spondylotic Myelopathy
Also known as "Spinal Cord Compression."
We have selected the following expert medical opinion based on its clarity, reliability and accuracy. Credits: Sourced from the website OrthoInfo, contributed and/or updated by Dr Nilesh M. Patel, and peer-reviewed by Dr Stuart J. Fischer and Dr Louis G. Jenis. Please refer to your own medical practitioner for a final perspective, assessment or evaluation.
What is cervical spondylotic myelopathy?
Cervical spondylotic myelopathy (CSM) is a neck condition that arises when the spinal cord becomes compressed—or squeezed—due to the wear-and-tear changes that occur in the spine as we age. The condition commonly occurs in patients over the age of 50.
Because the spinal cord carries nerve impulses to many regions in the body, patients with CSM can experience a wide variety of symptoms. Weakness and numbness in the hands and arms, loss of balance and coordination, and neck pain can all result when the normal flow of nerve impulses through the spinal cord is interrupted.
Anatomy
Your spine is made up of 24 bones, called vertebrae, that are stacked on top of one another.
The seven small vertebrae that begin at the base of the skull and form the neck comprise the cervical spine.
Cervical spondylotic myelopathy occurs in the cervical spine—the seven small vertebrae that form the neck:
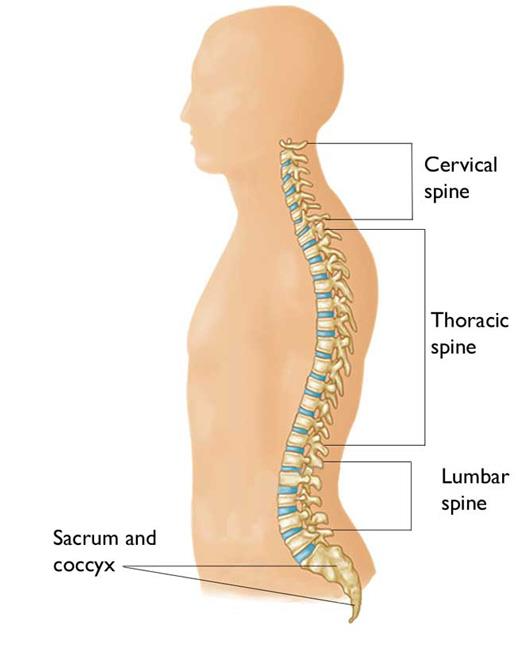
Other parts of your spine include:
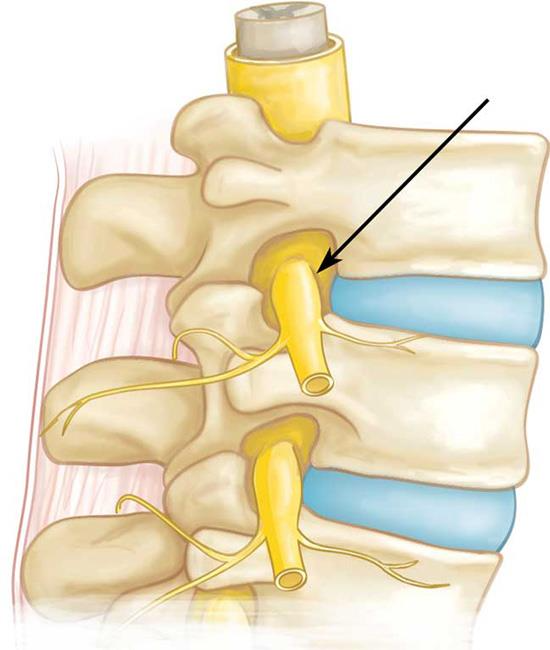
Spinal cord and nerves
The spinal cord extends from the skull to your lower back and travels through the middle part of each stacked vertebra, called the central canal. Nerves branch out from the spinal cord through openings in the vertebrae (foramen) and carry messages between the brain and muscles.
Spinal nerve root:
Intervertebral disks
In between your vertebrae are flexible intervertebral disks. They act as shock absorbers when you walk or run.
Intervertebral disks are flat and round and about a half inch thick.
They are made up of two components:
- Annulus fibrosus: This is the tough, flexible outer ring of the disk.
- Nucleus pulposus: This is the soft, jelly-like center of the disk.
Cause
Cervical spondylotic myelopathy (CSM) arises from degenerative changes that occur in the spine as we age. These degenerative changes in the disks are often called arthritis or spondylosis.
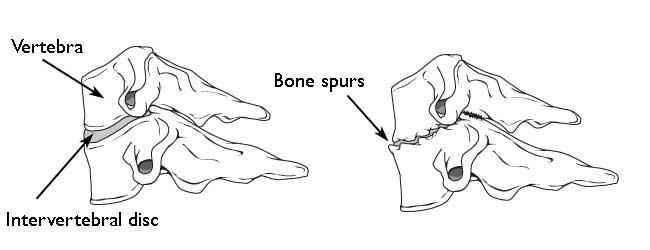
Cervical Disk Degeneration
Bone spurs
As the disks in the spine age, they lose height and begin to bulge. They also lose water content, begin to dry out, and become stiffer. This problem causes settling, or collapse, of the disk spaces and loss of disk space height.
As the disks lose height, the vertebrae move closer together. The body responds to the collapsed disk by forming more bone—called bone spurs—around the disk to strengthen it. These bone spurs contribute to the stiffening of the spine. They may also make the spinal canal narrow—compressing or squeezing the spinal cord.
(Left) Side view of a healthy cervical vertebra and disk. (Right) A disk that has degenerated and collapsed.
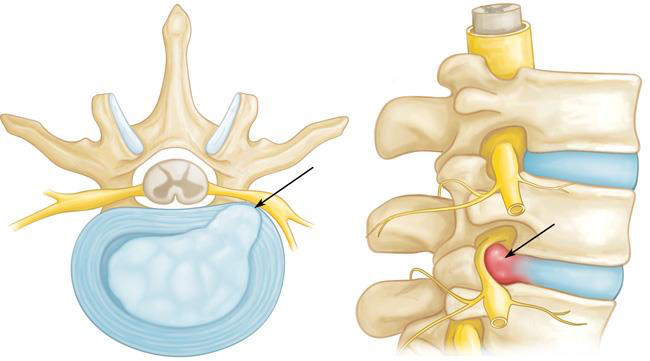
Herniated disk
A disk herniates when its jelly-like center (nucleus pulposus) pushes against its outer ring (annulus fibrosus). If the disk is very worn or injured, the nucleus may squeeze all the way through. When a herniated disk bulges out toward the spinal canal, it can put pressure on the spinal cord or nerve roots.
As disks deteriorate with age, they become more prone to herniation. A herniated disk often occurs with lifting, pulling, bending, or twisting movements.
Herniated disk (cross-section and side views):
Other Causes of Myelopathy
Myelopathy can arise from other conditions that cause spinal cord compression, as well. Although these conditions are not related to disk degeneration, they may result in the same symptoms as CSM.
Rheumatoid arthritis
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium, the thin membrane that lines the joints.
As the synovium swells, it may lead to pain and stiffness and, in severe cases, destruction of the facet joints in the cervical spine. When this occurs, the upper vertebra may slide forward on top of the lower vertebra, reducing the amount of space available for the spinal cord.
Injury
An injury to the neck—such as from a car accident, sports, or a fall—may also lead to myelopathy.
For example, a "rear end" car collision may result in hyperextension, a backward motion of the neck beyond its normal limits, or hyperflexion, a forward motion of the neck beyond its normal limits. Because these types of injuries often affect the muscles and ligaments that support the vertebrae, they may lead to spinal cord compression.
Symptoms
Typically, the symptoms of CSM develop slowly and progress steadily over several years. In some patients, however, the condition may worsen more rapidly.
Patients with CSM may experience a combination of the following symptoms:
- Tingling or numbness in the arms, fingers, or hands
- Weakness in the muscles of the arms, shoulders, or hands. You may have trouble grasping and holding on to items.
- Imbalance and other coordination problems. You may have trouble walking or you may fall down. With myelopathy, there is no sensation of spinning, or "vertigo." Rather, your head and eyes feel steady, but your body feels unable to follow through with what you are trying to do.
- Loss of fine motor skills. You may have difficulty with handwriting, buttoning your clothes, picking up coins, or feeding yourself.
- Pain or stiffness in the neck
Doctor Examination
Physical Examination
After discussing your medical history and general health, your doctor will ask you about your symptoms.
He or she will conduct a thorough examination of your neck, shoulders, arms, hands, and legs, looking for:
- Changes in reflexes—including the presence of hyper-reflexia,a condition in which reflexes are exaggerated or overactive
- Numbness and weakness in the arms, hands, and fingers
- Trouble walking, loss of balance, or weakness in the legs
- Atrophy—a condition in which muscles deteriorate and shrink in size
Tests
X-rays
These provide images of dense structures, such as bone. An x-ray will show the alignment of the vertebrae in your neck.
Magnetic resonance imaging (MRI) scans
These studies create better images of the body's soft tissues. An MRI can show spinal cord compression and help determine whether your symptoms are caused by damage to soft tissues—such as a bulging or herniated disk.
This MRI image shows herniated disks pressing on the spinal cord (red arrows):
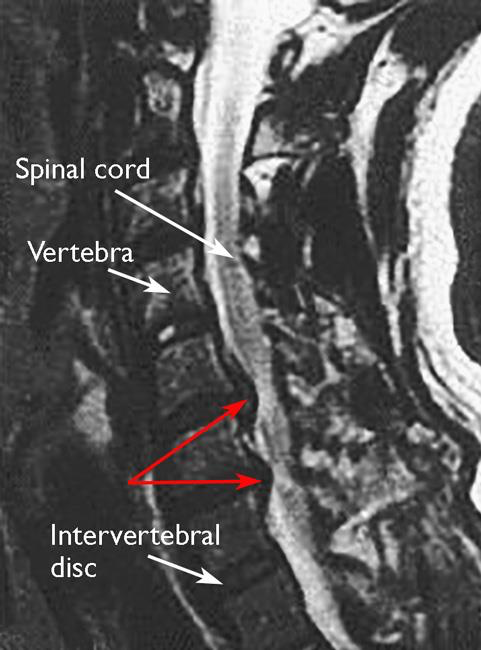
Reproduced from Boyce R, Wang J: Evaluation of neck pain, radiculopathy and myelopathy: imaging, conservative treatment, and surgical indications. Instructional Course Lectures 52. Rosemont, IL, American Academy of Orthopaedic Surgeons, 2003, pp.489-495.
Computed tomography (CT) scans
More detailed that a plain x-ray, a CT scan can show narrowing of the spinal canal and can help your doctor determine whether you have developed bone spurs in your cervical spine.
This CT scan shows bone spurs that have led to narrowing of the spinal canal (arrows):

Myelogram
This is a special type of CT scan. In this procedure, a contrast dye is injected into the spinal column to make the spinal cord and nerve roots show up more clearly.
Treatment
Nonsurgical Treatment
In milder cases, initial treatment for CSM may be nonsurgical. The goal of nonsurgical treatment is to decrease pain and improve the patient's ability to perform daily activities.
Nonsurgical treatment options include:
Soft cervical collar
This is a padded ring that wraps around the neck and is held in place with velcro. Your doctor may advise you to wear a soft cervical collar to allow the muscles of the neck to rest and limit neck motion. A soft collar should only be worn for a short period of time since long-term wear may decrease the strength of the muscles in your neck.
Physical therapy
Specific exercises can help relieve pain, strengthen neck muscles, and increase flexibility. Physical therapy can also help you maintain strength and endurance so that you are better able to perform your daily activities. In some cases, traction can be used to gently stretch the joints and muscles of the neck.
Medications
In some cases, medications can help improve your symptoms:
- Nonsteroidal anti-inflammatory medications (NSAIDs): Drugs like aspirin, ibuprofen, and naproxen can help relieve pain from reduce inflammation.
- Oral corticosteroids: A short course of oral corticosteroids may help relieve pain by reducing inflammation.
- Epidural steroid injection: Although not often used to treat CSM, in this procedure, steroids are injected into the space next to the covering of the spinal cord (the "epidural" space) to help reduce local inflammation. Although a steroid injection may temporarily help relieve pain and swelling, it will not relieve pressure on the spinal cord.
- Narcotics: These medications are reserve for patients with severe pain that is not relieved by other options. Narcotics are usually prescribed for a limited time only.
Although people sometimes turn to chiropractic manipulation for neck and back pain, manipulation should never be used for spinal cord compression.
Surgical Treatment
If nonsurgical treatment does not relieve your symptoms, your doctor will talk with you about whether you would benefit from surgery. The majority of patients with symptoms and tests consistent with CSM are recommended to have surgery.
There are several procedures that can be performed to help relieve pressure on the spinal cord. The procedure your doctor recommends will depend on many factors, including what symptoms you are experiencing and the levels of the spinal cord that are involved.
_______________________________________________________________________________________________________________________
Are you a healthcare practitioner who enjoys patient education, interaction and communication?
If so, we invite you to criticise, contribute to or help improve our content. We find that many practicing doctors who regularly communicate with patients develop novel and often highly effective ways to convey complex medical information in a simplified, accurate and compassionate manner.
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical expertise between doctors and patients. We support collaboration, as opposed to competition, between all members of the healthcare profession and are striving towards the provision of peer reviewed, accurate and simplified medical information to patients. Please share your unique communication style, experience and insights with a wider audience of patients, as well as your colleagues, by contributing to our digital platform.
Your contribution will be credited to you and your name, practice and field of interest will be made visible to the world. (Contact us via the orange feed-back button on the right).
Disclaimer:
MedSquirrel is a shared knowledge, collective intelligence digital platform developed to share medical knowledge between doctors and patients. If you are a healthcare practitioner, we invite you to criticise, contribute or help improve our content. We support collaboration among all members of the healthcare profession since we strive for the provision of world-class, peer-reviewed, accurate and transparent medical information.
MedSquirrel should not be used for diagnosis, treatment or prescription. Always refer any questions about diagnosis, treatment or prescription to your Doctor.
